Lancet Respirat Med:肺内微生物群状况可预测肺移植患者预后!
2021-01-18 MedSci原创 MedSci原创
在慢性肺部疾病中常见呼吸微生物群改变,与肺功能下降有关,还与疾病进展有关。肺移植后呼吸微生物群变化的临床意义,特别是与慢性肺同种异体移植功能障碍(CLAD)的发展有关的临床意义尚不清楚。本研究旨在评估
在慢性肺部疾病中常见呼吸微生物群改变,与肺功能下降有关,还与疾病进展有关。肺移植后呼吸微生物群变化的临床意义,特别是与慢性肺同种异体移植功能障碍(CLAD)的发展有关的临床意义尚不清楚。本研究旨在评估健康肺移植受者的肺微生物群特征对随后无CLAD存活预后的影响。
研究人员回顾性分析了一组在密西根大学进行肺移植的无症状患者移植术后1年内肺泡灌洗液(BALF)的微生物特征。主要终点是500天内的CLAD或死亡的综合评估。主要的微生物预测变量是细菌DNA负荷(总16S rRNA基因拷贝数/mL)和微生物群组成。
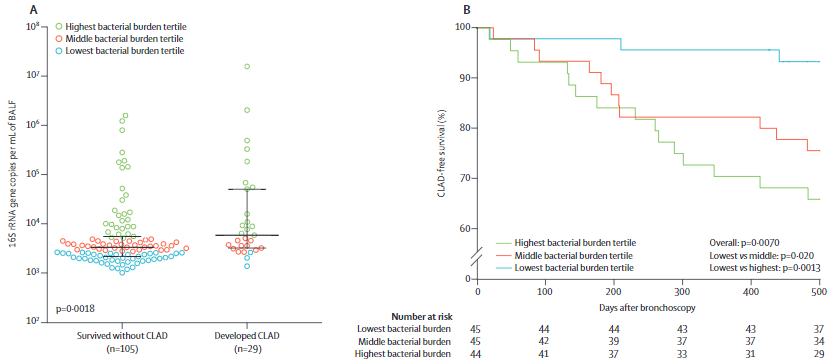
2005年10月21日-2017年8月25日,共分析了134位患者的BALF。从BALF采样开始的500天内,有24位(18%)患者发展为CLAD,5位(4%)患者在确诊CLAD前死亡,另105位(78%)完成了随访且未发生CLAD。
肺移植后肺细菌负荷增加预示慢性排斥和死亡
经人口和临床因素控制后,肺细菌负荷可预测支气管镜检查监测500天内CLAD或死亡发展。当将细菌负荷作为连续变量或三分位数进行分析时,上述相关性显著(作连续变量:负荷每增加log10,风险比[HR] 2.49;三分位数:与最低三分位数相比,中间和最高三分位数的HR分别是4.94和10.56)。
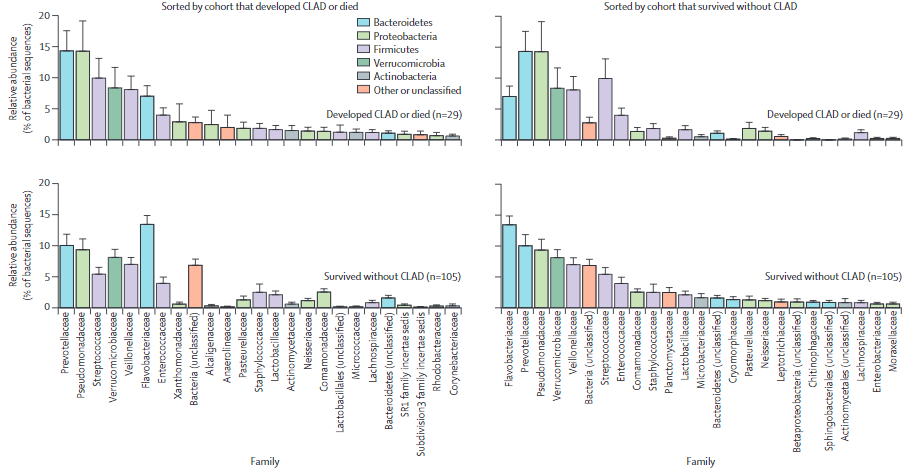
不同状况患者肺微生物组成不同
发生CLAD或死亡的患者,肺微生物群的组成与幸存患者和未发生CLAD患者的明显不同。无单个细菌分类群被确认与CLAD的发生或死亡相关。
在肺移植后1年内无症状的患者中,肺细菌负荷增加提示慢性排斥和死亡。肺部微生物群是克服同种异体移植功能障碍的一个尚未被研究且有望攻克的危险因素。
原始出处:
Michael P Combs, et al. Lung microbiota predict chronic rejection in healthy lung transplant recipients: a prospective cohort study. The Lancet Respiratory Medicine. January 15, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Lancet#
104
#微生物#
73
#患者预后#
76
#微生物群#
92
#Med#
85
顶刊就是不一样,质量很高,内容精彩!学到很多
126