Science:小分子药物MYK-461可阻止和逆转肥厚性心肌病
2016-02-06 MedSci 生物谷
MyoKardia公司作为一家开创精准医疗治疗遗传性心血管疾病的生物制药公司2月4日宣布在Science期刊上发表了一篇论文,论文标题为“A Small-Molecule Inhibitor of Sarcomere Contractility Suppresses Hypertrophic Cardiomyopathy in Mice”。这篇论文证实作为该公司的候选先导药物(lead drug
MyoKardia公司作为一家开创精准医疗治疗遗传性心血管疾病的生物制药公司2月4日宣布在Science期刊上发表了一篇论文,论文标题为“A Small-Molecule Inhibitor of Sarcomere Contractility Suppresses Hypertrophic Cardiomyopathy in Mice”。这篇论文证实作为该公司的候选先导药物(lead drug candidate),MYK-461能够预防和逆转多种肥厚性心肌病(hypertrophic cardiomyopathy, HCM)模式基因突变小鼠的疾病发展。这项研究成果是MyoKardia公司、哈佛大学医学院、科罗拉多大学和斯坦福大学的合作结晶。这些数据进一步提供实验室和临床研究证据证实MYK-461有潜力作为一种重要的新方法治疗HCM。
MyoKardia公司首席医疗官Jonathan Fox博士说,“这些数据鼓舞人心,因为它们在生物化学、细胞和整体动物水平上展现出MYK-461有效地降低HCM基因突变后果。将这些发现从小鼠转移到人类,可能有巨大潜力改善患有这种破坏性疾病的病人的生命。”
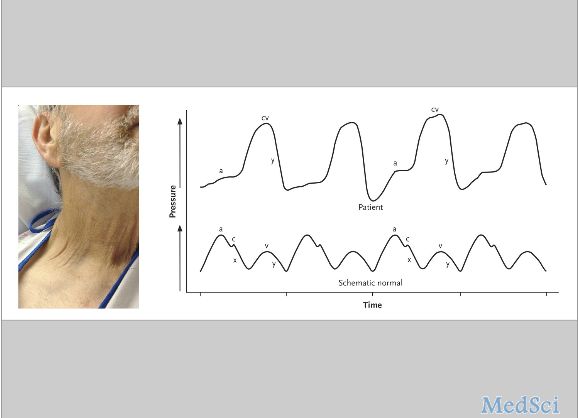
为了研究肌节中的基因突变在HCM产生中的作用,MyoKardia公司使用之前培育出的HCM模式小鼠,这些小鼠表现出人HCM的关键性形态和功能特征。为了量化左心室肥大---HCM的主要特征---的程度,研究人员非侵入式地测量了左心室壁厚度(left ventricular wall thickness, LVWT)。
MyoKardia公司研究人员和他们的合作伙伴证实早期和长期服用MYK-461可阻止这种疾病的发展。相比于未接受治疗的基因突变小鼠中观察到的LVWT增加,在接受MYK-461治疗的基因突变小鼠中并未观察到LVWT增加。这项研究还证实一旦服用MYK-461,它能促进这种疾病的部分逆转,这点可从已产生心肌肥大的HCM模式小鼠中测量到的LVWT下降加以证明。再者,这项研究还发现MYK-461可阻止左室纤维化产生。左室纤维化是HCM的一种重要的组织病理学特征,其他具有潜在危险性的心脏病也涉及这一特征。
MyoKardia公司首席执行官Tassos Gianakakos说,“这些发现让我们备感鼓舞,它们支持我们的治疗假设:降低心肌收缩性能够阻止或逆转结构和功能上的异常,正是这些异常导致折磨着HCM病人的症状。我们认为在临床开发上,MYK-461是第一个获得这些效果的药物。这种方法可能代表着一个治疗遗传性心肌病的更为一般性的范例,可能让我们更接近于我们的最终目标,也就是改善患有这种衰竭性疾病的病人及其家属的生命。”
MyoKardia公司当前正在I期临床试验中评估MYK-461。这项临床试验旨在评估MYK-461的安全性和耐受性,并预计会提供它的药代动力学和药效动力学方面的数据。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










希望早日用上myk461
101
#小分子#
61
非常有用
148
已分享,热议
139
#SCIE#
58
#肌病#
55
有用
149
沉默基因
141