JACC:儿童时期二手烟的暴露增加了房颤的发生风险
2019-09-24 佚名 MedSci原创
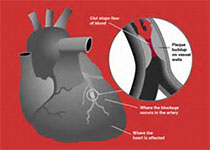
吸烟可以增加房颤发生风险,近期的一项横断面研究显示父母吸烟同样是一个危险因素。本研究的目的旨在评估父母吸烟是否会增加子代房颤风险。 本研究纳入了2816名Framingham心脏研究队列中的子代,其中82%暴露与父母的吸烟状态中,父母吸烟每日增加一包,子代房颤的发生风险增高18%( [HR]: 1.18; 95% [CI]: 1.00-1.39; p = 0.04),另外,父母吸烟也是子代吸
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#儿童时期#
87
#JACC#
122
#ACC#
111
#二手烟#
93