医生必看!全身各区域淋巴结 CT 图谱
2016-07-28 子弹头 肿瘤时间
这篇发表在 Radiology 杂志上的经典文章系统归纳了在常规 CT 情况下如何确定全身各区域淋巴结,并且给出了非常清晰的图谱。一起来回顾下吧。基本定位(点击图片可查看大图)注:左、左下、右、右中、右下依次是:头颈部、胸部、腹部、男性盆腔、女性盆腔的定位像。头颈部定位像 hn01-hn09 层面的 CT 影像 (上中颈)注:PSL 副鼻窦淋巴,PAuN 耳前淋巴结,MN 乳突淋巴结,NL 鼻咽
这篇发表在 Radiology 杂志上的经典文章系统归纳了在常规 CT 情况下如何确定全身各区域淋巴结,并且给出了非常清晰的图谱。一起来回顾下吧。
基本定位(点击图片可查看大图)
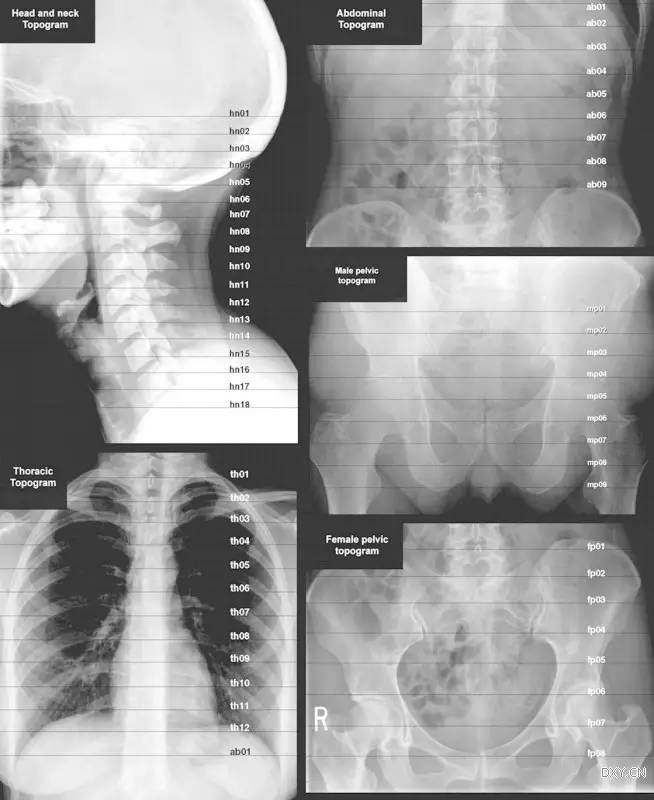
注:左、左下、右、右中、右下依次是:头颈部、胸部、腹部、男性盆腔、女性盆腔的定位像。
头颈部定位像 hn01-hn09 层面的 CT 影像 (上中颈)
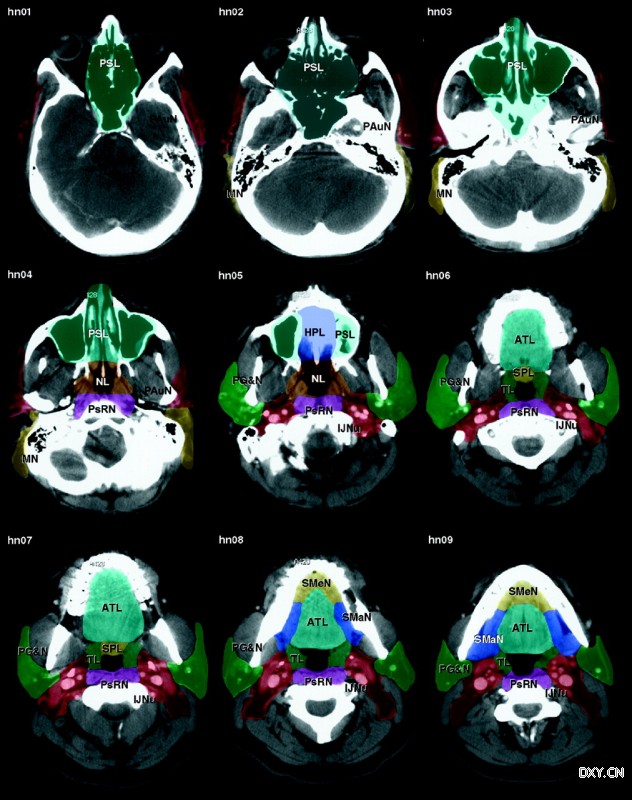
注:PSL 副鼻窦淋巴,PAuN 耳前淋巴结,MN 乳突淋巴结,NL 鼻咽淋巴丛,PsRN 上咽后壁淋巴结,HPL 硬腭淋巴丛,IJNu 上颈内淋巴结,PG&N 腮腺和淋巴结,ATL 舌前淋巴腺,SPL 软腭淋巴,TL 扁桃体淋巴丛,SMaN下颌下淋巴结,SMeN颏下淋巴结
头颈部定位像 hn10-hn18 层面的 CT 影像(下颈部,锁骨上)
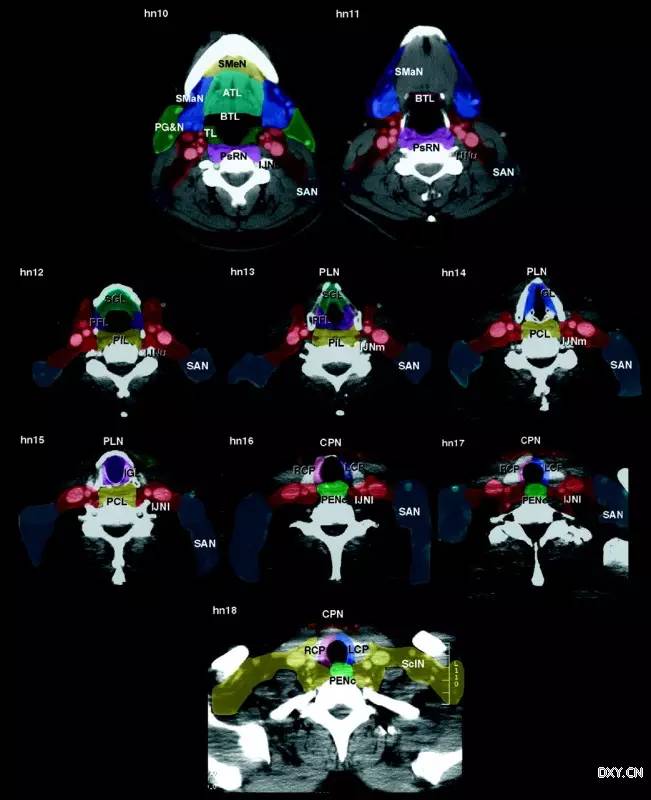
注:BTL 舌根淋巴结,SAN 脊髓副淋巴结,SGL 声门上淋巴丛,PFL 梨状窝淋巴腺,IJNm 颈内静脉淋巴结,PiL 下咽后壁淋巴结 ,PLN喉前淋巴结,IGL 声门下淋巴丛,PCL 环后区淋巴结,IJN 颈内淋巴结,RCP 右颈气管旁淋巴结,LCP 左颈气管旁淋巴结,PEN 食管旁淋巴结,CPN 颈部气管前淋巴结,ScIN 锁骨上淋巴结
胸部定位 CT 像(纵膈)
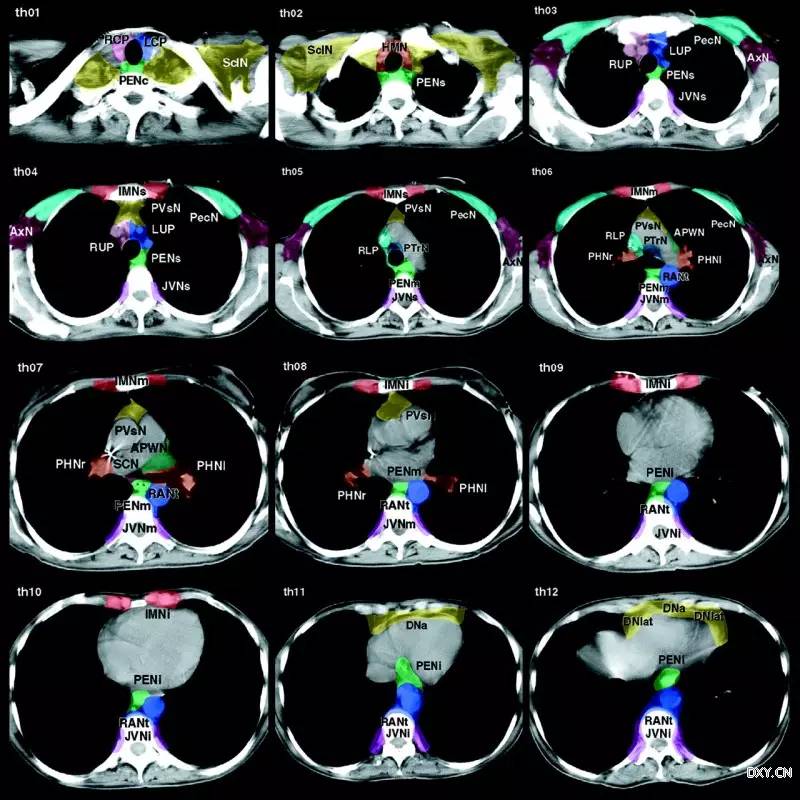
注:HMN 上纵隔淋巴结,RUP 右上气管旁淋巴结,LUP 左上气管旁淋巴结,JVN 胸椎旁淋巴结,PecN 胸肌淋巴结,AxN 腋窝淋巴结,IMN 内乳淋巴结,PVsN 血管前淋巴结,PTrN 纵隔气管前淋巴结,PHN (肺)门淋巴结,APWN 主肺动脉窗淋巴结,RAN 主动脉旁淋巴结,SCN 隆突下淋巴结,DNa 横膈淋巴结
腹部定位 CT 像
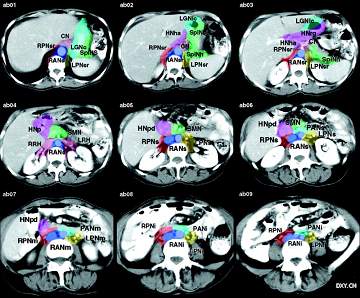
注:CN 腹腔干淋巴结,RPN 右主动脉旁淋巴结,LGN 胃左淋巴结,SplN 脾淋巴结,LPN 左主动脉旁淋巴结,HN 肝淋巴结,RRH 右肾门淋巴结,LRH 左肾门淋巴结,SMN 肠系膜上淋巴结,RAN 主动脉旁淋巴结,PAN主动脉前淋巴结
男性盆腔定位 CT 像
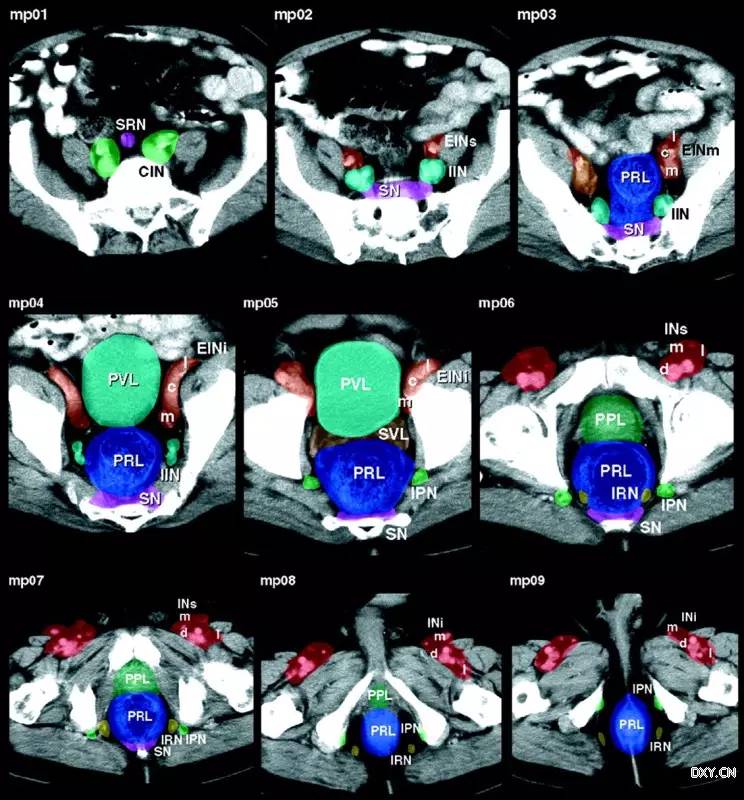
注:SRN 直肠上淋巴结,CIN 髂总淋巴结,SN 骶骨淋巴结,EIN 髂外淋巴结,IIN 髂内淋巴结,PRL 直肠旁淋巴丛,PVL 膀胱周淋巴丛,IPN 阴部内淋巴结,SVL 精囊淋巴结,INs 腹股沟浅淋巴结,PPL 前列腺周淋巴丛,IRN 直肠下淋巴结
女性盆腔定位 CT 像
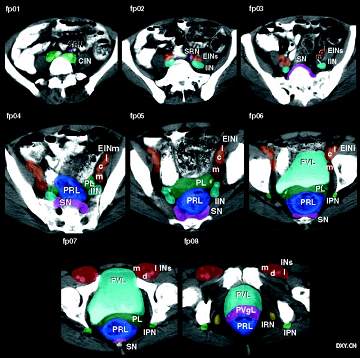
注:PL 子宫旁淋巴丛,PVgL 阴道旁淋巴丛
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











很好,不错,以后会多学习
114
很好,不错,以后会多学习
94
很好,不错,以后会多学习
144
继续学习
89
继续关注
112
值得学习
57
好文章,谢谢分享学习了
69
要是能给出文章出处就好了
126
好好学习,这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
85
#淋巴结#
102