Prostate:在前列腺癌中,MCM10的过表达能够促进细胞的增殖和预测不良预后
2018-08-15 AlexYang MedSci原创
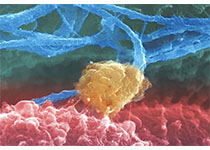
前列腺癌(PCa)是男性泌尿生殖系统中最常见的恶性肿瘤之一。鉴定新的PCa生物标记十分紧迫和必要。最近,有研究人员通过分析公共数据库评估了MCM10在前列腺癌中的表达水平。进一步的是,研究人员进行了功能缺失试验分析来评估MCM10对细胞增殖、细胞凋亡和克隆形成的影响。更多的是,研究人员还利用基因芯片和生物信息学分析探索了MCM10潜在的作用机制。研究发现,他们首次阐释了MCM10在PCa中表达是显
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#过表达#
68
前列腺增生微创治疗。
120
前列腺癌靶向药物治疗。
91
#不良预后#
73
#ROS#
65
#PRO#
68