分子检测越来越广泛地用于甲状腺结节(特别是不确定类别)良恶性鉴定。血浆中无细胞DNA(cfDNA)水平已用于诊断其他器官/组织的癌症。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究对甲状腺结节患者的cfDNA水平进行评估,并以明确用于识别恶性肿瘤的临界值。
研究人员对甲状腺结节患者进行超声检查(USG)和USG指导的细针穿刺术(FNA)检查,并在需要时进行手术。研究人员从受试者血浆中提取无细胞的DNA并进行定量。在初步分析(确定临界值)中,研究人员比较了Bethesda 2级患者和Bethesda 5-6级患者的cfDNA水平,以确定可区分恶性结节与良性结节的临界值。在随后的分析中,研究人员对不确定结节的患者应用上述截止值(截止值验证)以评估预测恶性肿瘤的能力。
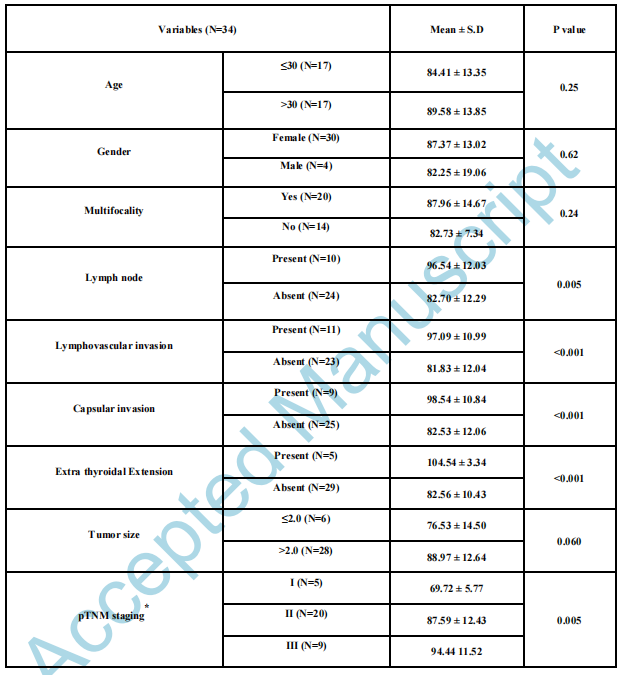
研究人员进行了FNA(n=119)及组织病理学检查,Bethesda 2患者(n=69)和Bethesda 5-6患者( n=13)。两组患者的无细胞DNA分别为22.85±1.27和96.20±8.31(ng/ml)。cfDNA临界值为67.9 ng/ml,AUC为0.992(95%CI为0.97-1.0),其灵敏度为100%,特异性为93%,可用于识别恶性病变。不确定的(Bethesda 3和4)甲状腺结节患者进行了手术(恶性n=24),(良性n=13),并且使用先前确定的cfDNA临界值,研究人员能够以100%的敏感性和92.3%的特异性识别出恶性病变。基于cfDNA的分类与基于组织病理学检查的良性和恶性结节分类的结果一致(Cohen’s kappa指数为0.94,p<0.001)。
由此可见,血浆cfDNA可以帮助区分恶性和良性甲状腺结节。
原始出处:
Susmita Dutta.et al.Plasma cell free DNA to differentiate malignant from benign thyroid nodules.JCEM.2021.https://doi.org/10.1210/clinem/dgab030
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JCEM#
61
#JCE#
86
好
125
好
121