Leukemia:iFCG化疗方案治疗携带IGHV突变且无TP53突变的慢性淋巴细胞白血病
2021-06-12 xiaozeng MedSci原创
目前联合氟达拉滨(fludarabine)、环磷酰胺(cyclophosphamide)和利妥昔单抗(rituximab)(FCR)的化学免疫疗法(CIT)已成为慢性淋巴细胞白血病(CLL)患者的标准
目前联合氟达拉滨(fludarabine)、环磷酰胺(cyclophosphamide)和利妥昔单抗(rituximab)(FCR)的化学免疫疗法(CIT)已成为慢性淋巴细胞白血病(CLL)患者的标准治疗策略。
德克萨斯大学MD安德森癌症中心(MDACC)的一项初始II期临床研究显示,FCR一线治疗的总体反应率为95%。然而,FCR治疗相关骨髓增生异常综合征(MDS)/急性髓系白血病(AML)的发病风险为2-5%。
因此,急需确定从CIT中获益最大的患者亚组。而在MDACC的FCR一线试验的长期随访表明,携带IGHV突变的亚组的患者10年PFS约为 55%,且在大约8年后出现平台期,这也说明这些CLL患者的可能会完全治愈。
该研究是一项针对先前未经治疗的携带IGHV突变且不存在del(17p)/TP53突变的CLL患者的II期临床试验。在该研究中,患者主要接受了三个周期的依鲁替尼(ibrutinib)、氟达拉滨、环磷酰胺和阿托珠单抗(obinutuzumab)(iFCG)治疗。
达到完全缓解(CR)的、CR且计数不完全恢复(CRi)的以及骨髓无法检测到可测量残留疾病(U-MRD)的患者接受额外的9个周期的依鲁替尼和3个周期的阿托珠单抗治疗;而所有其他患者则接受额外的9个周期的依鲁替尼和阿托珠单抗治疗。而在第12周期后骨髓U-MRD缓解的患者停止所有包括依鲁替尼在内的治疗。
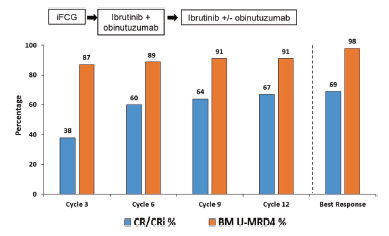
研究流程图
结果显示,总共有45名患者接受了治疗,患者的中位随访时间为41.3个月。在所有患者中,治疗三个周期后,38%的患者达到CR/CRi,87%达到骨髓U-MRD。在治疗第12个周期后,相应的患者比例为67%和91%。
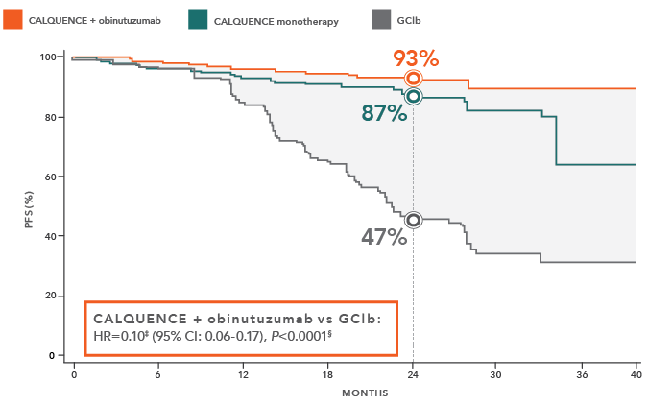
总体而言,44/45(98%)的患者达到了骨髓U-MRD的最佳反应。并无患者出现CLL的进展。患者的3年无进展生存率(PFS)和总生存率(OS)分别为98%和98%。所有完成12个周期治疗的患者均停用了依鲁替尼。在 58%和 40%的患者中分别出现3-4级中性粒细胞减少症和血小板减少症。
对治疗的响应
总而言之,该研究结果揭示,仅3个周期的iFCG化疗方案对于携带IGHV突变且无del(17p)/TP53突变的CLL患者来说是一种有效的限时治疗方案。
原始出处:
Jain, N., Thompson, P., Burger, J. et al. Ibrutinib, fludarabine, cyclophosphamide, and obinutuzumab (iFCG) regimen for chronic lymphocytic leukemia (CLL) with mutated IGHV and without TP53 aberrations. Leukemia (18 May 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#IGHV#
59
#淋巴细胞白血病#
50
#淋巴细胞#
56
#p53#
82
#TP53#
113
学习了,权威!
95
学习了!
89