Nat Commun:限制进食时间可以降低绝经后乳腺癌的概率
2021-01-26 haibei MedSci原创
TRF在没有限制卡路里或减轻体重的情况下,抑制了两个模型中肥胖增强的乳腺肿瘤生长。TRF还可以减少乳腺癌向肺部的转移。
肥胖症是世界范围内的一个严重的健康威胁,在过去的三十年里,肥胖症和代谢综合征的发病率已经上升到了流行病的水平,特别是在西方国家。肥胖及其相关的代谢失调是2型糖尿病、心脏和肾脏疾病,以及至少有13种癌症,包括绝经后乳腺癌、结直肠癌、子宫内膜癌、食管腺癌和胆囊癌的风险因素。最近的研究表明,肥胖和乳腺癌有很强的关联性。
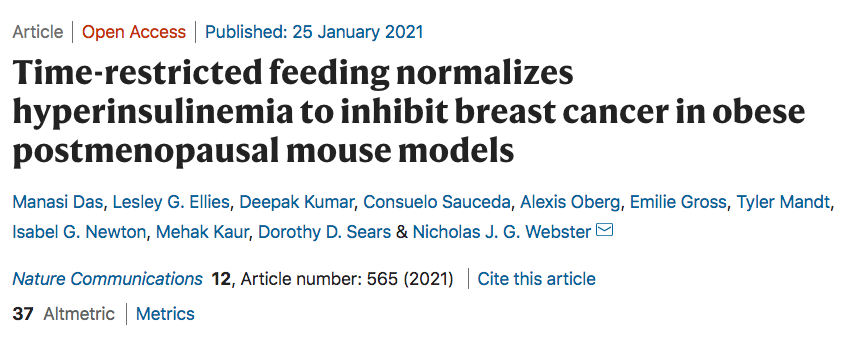
已有的研究显示,热量限制可以改善肥胖相关的有害代谢影响,并抑制癌症的进展,但该干预措施在临床之外难以实施和维持。最近在Nature Communications发表的一项研究中,研究人员在肥胖驱动的绝经后乳腺癌小鼠模型上测试时间限制喂养(TRF)的方法。研究结果表明,TRF在没有限制卡路里或减轻体重的情况下,抑制了两个模型中肥胖增强的乳腺肿瘤生长。TRF还可以减少乳腺癌向肺部的转移。
此外,在肿瘤基因模型小鼠中,TRF可以在肥胖发生前延迟了肿瘤的发生。值得注意的是,TRF增加了全身胰岛素的敏感性,降低了高胰岛素血症,恢复了肿瘤的昼夜基因表达节律,并减轻了肿瘤的生长和胰岛素信号传导。
重要的是,用二氮唑抑制胰岛素分泌可模拟TRF,而通过植入胰岛素泵人工升高胰岛素可逆转TRF的作用,说明TRF是通过调节高胰岛素血症发挥作用的。
因此,这些数据表明,TRF在乳腺癌的预防和治疗中可能是有效的。
原始出处:
Manasi Das et al. Time-restricted feeding normalizes hyperinsulinemia to inhibit breast cancer in obese postmenopausal mouse models. Nature Communications (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
96
#COMMUN#
81
#绝经#
94
#进食#
78
#绝经后#
95