SCI TRANSL MED:淋巴瘤靶向治疗新突破
2017-06-30 cailingrui MedSci原创
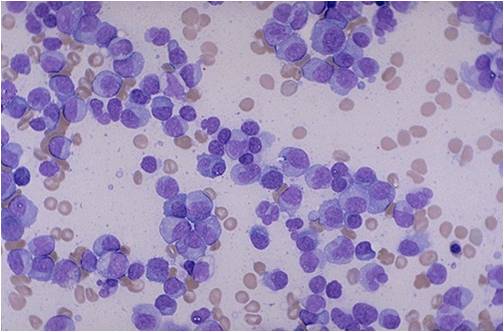
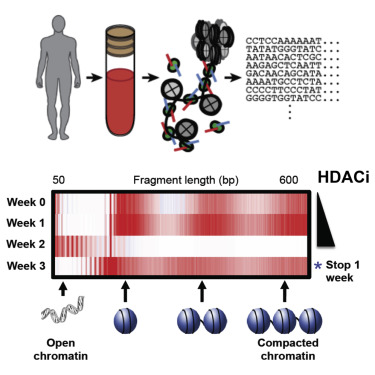
作者研究了由SESTRIN1缺失导致的肿瘤发生机制,确定了SESTRIN1和EZH2之间的机械连接,这种机械连接本质上是一种表观遗传修饰,并在多个癌症类型中扮演重要角色。研究人员证明了靶向EZH2的有效性取决于SESTRIN1的遗传和表观遗传状态,并且还报道了EZH2上的突变可以使癌细胞对其他靶向治疗敏感。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Transl#
58
#新突破#
75
#TRA#
56
#Med#
57