毫无征兆突发心梗并不罕见
2017-10-15 许珈 澎湃新闻
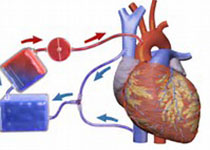
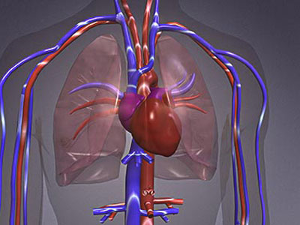
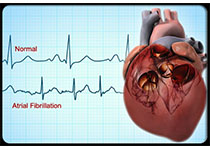
40岁男性因胸痛前往医院,初步判断是急性广泛前壁心梗,此前并无心脏病史,经过造影确认前降支近端完全闭塞。“我们立即就做了支架植入,手术过程中病人血管情况都可以通过DSA血管造影系统看到。仅仅19分钟我们就把血管打通了,毫无疑问这种诊断和治疗相结合,大大缩短了危重病人的救治时间。” 上海市第六人民医院心血管内科主任沈成兴说。如今,像这样没有预兆的心梗患者并不罕见。心血管内科主任医师陆志刚透露, 10
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习了谢谢作者分享!
122
不错的文章值得一读.
88
谢谢分享
86
#罕见#
70
学习一下知识了
79
学习了很多先进的医疗技术
160
造成急性胸痛的原因很复杂.大约有30%的患者是突发急性心梗.而发病初期的6小时被视为救治[黄金时间".
0
不错的文章值得一读.
104