Science子刊:科学家找到针对饮食失调和肥胖症的新途径
2021-04-26 Sunny MedSci原创
在老鼠身上进行的这项研究提供了初步的证据,证明操纵MC3R可以刺激或抑制食物摄入。
 breathelifehealingcenters
breathelifehealingcenters
科学家已经确定了治疗肥胖和进食障碍(例如神经性厌食症)的潜在药物靶标,目前尚无治疗方法。
已知下丘脑AgRP(Agouti相关蛋白)神经元的消融会导致致命的厌食症,而它们的激活会刺激贪婪的进食并抑制其他动机状态,包括恐惧和焦虑。尽管AgRP神经元在双向控制进食方面发挥着关键作用,但目前还没有专门针对这一回路的治疗方法。
在《科学转化医学》(Science Translational Medicine)杂志上发表的一项新研究中,密歇根大学和范德比尔特大学的一组研究人员指出了一种名为melanocortin 3受体(MC3R)的蛋白质,它是进入大脑电路的途径,该大脑电路控制着人体的能量平衡和食物摄入。

在老鼠身上进行的这项研究提供了初步的证据,证明操纵MC3R可以刺激或抑制食物摄入。
MC3R位于神经元的表面,在该处发送和接收有关体内总体能量平衡的信号。尽管这种蛋白质遍布整个大脑,但在控制老鼠和人类进食的大脑区域中尤为普遍。
研究结果显示,MC3R在多个脑区表达,并在小鼠和人类的一些区域表现出性双态表达。MC3R的缺失产生了多种形式的性双态厌食症,与人类神经性厌食症的各个方面相似。然而,在AgRP神经元中,MC3R的表达没有性别差异,其中97%的神经元表达MC3R。弧形MC3R神经元的化学遗传学操作和MC3R的药理学操作分别对雄性和雌性小鼠的摄食行为发挥了有效的双向调节作用,而表达MC3R的细胞的全面消融产生了致命的厌食症。MC3R化合物对摄食的药理作用取决于小鼠体内完整的AgRP回路。
因此,MC3R的主导作用似乎是调节雄性和雌性小鼠的AgRP回路,其中性双态位点在摄食行为中发挥专门和从属的作用。
也就是说,MC3R是以厌食为特征的疾病的一个潜在治疗目标,也是减肥治疗的一个潜在目标。
UM生命科学研究所的神经科学家Patrick Sweeney表示,该大脑的两个主要区域接收有关体重和能量平衡的所有外围信息:下丘脑和脑干。研究发现,MC3R在下丘脑中表达最多,我们认为它在调节控制食物摄入的整个神经元回路中起着主导作用。
当能量储存过高时,MC3R从下丘脑的这个位置接收激素信号,并激活抑制食物摄入的神经回路。相反,该受体也可以感觉到人体需要更多的能量并激活刺激食物摄入的途径。
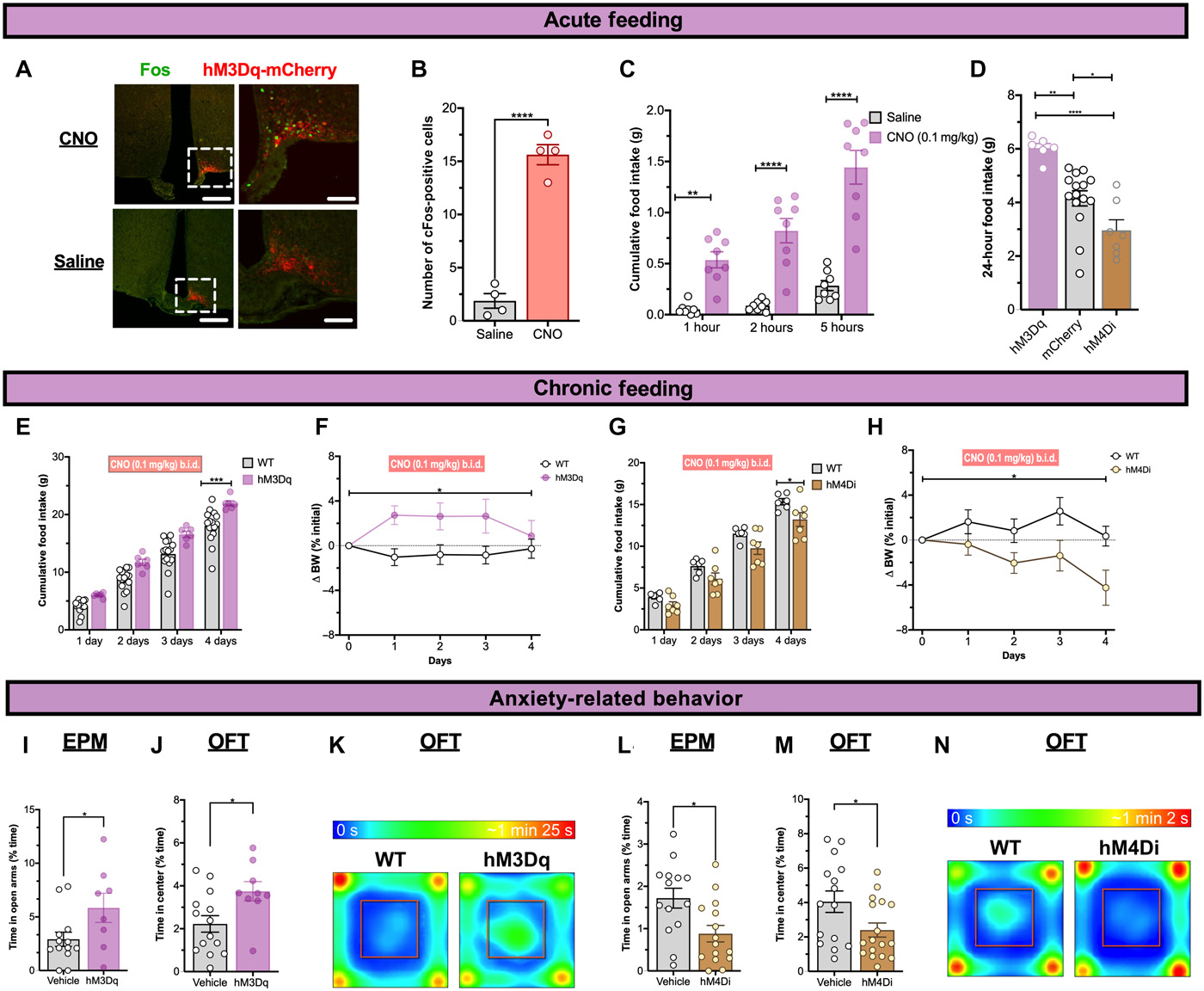 ARH MC3R神经元激活增加进食并减少焦虑
ARH MC3R神经元激活增加进食并减少焦虑
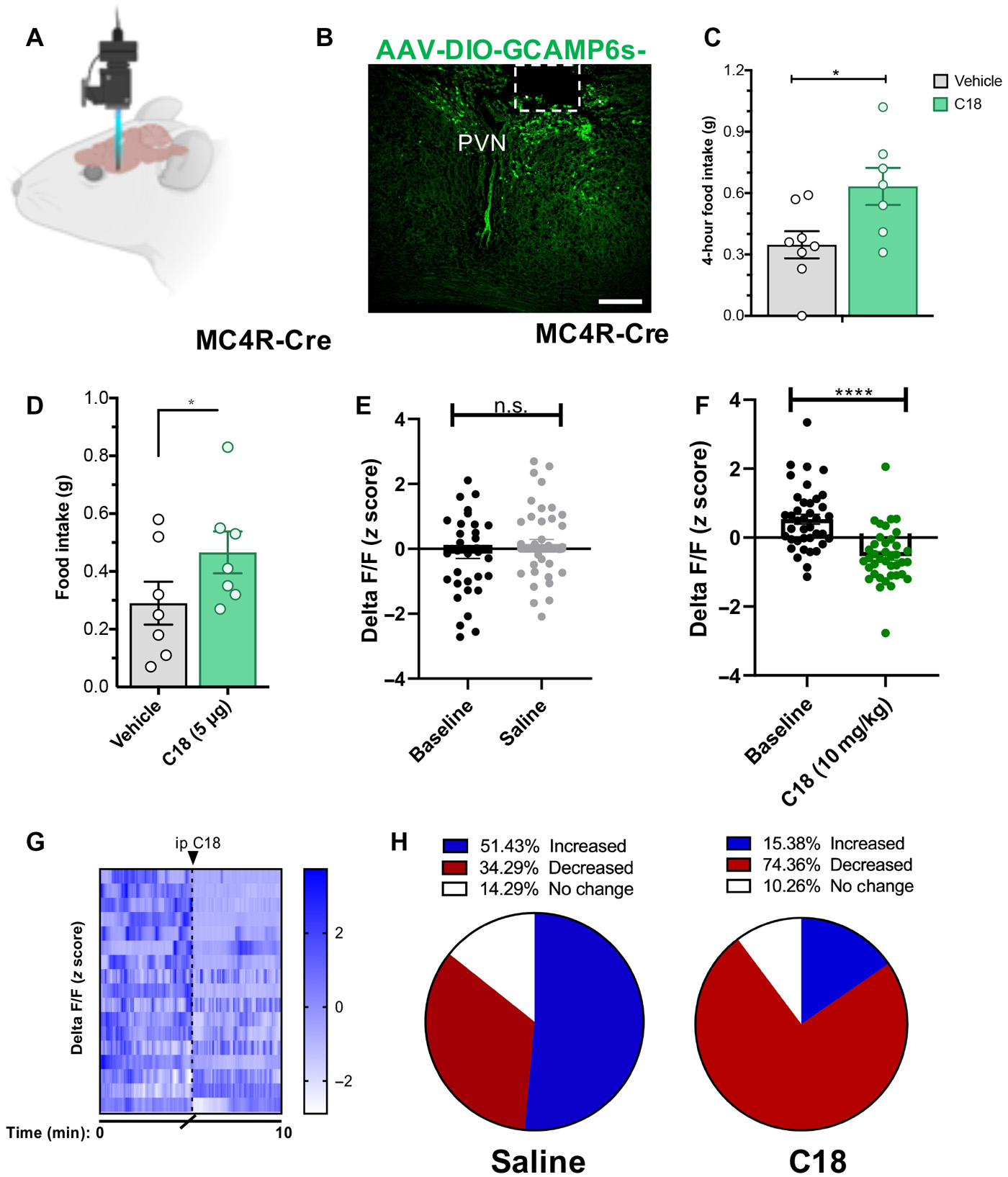 MC3R激动作用在体内抑制PVN MC4R神经元
MC3R激动作用在体内抑制PVN MC4R神经元
对于这项研究,研究人员检查了缺少MC3R蛋白的小鼠的行为和喂养反应。他们发现小鼠表现出与厌食症人类相同的许多特征。在某些情况下,雄性和雌性小鼠的行为反应差异很大-类似于人类的差异,在人类中,大约90%的神经性厌食症被诊断为雌性。
研究小组还确定,操作MC3R可以在两个方向上改变喂养习惯。当研究人员用刺激蛋白质活性的化合物处理小鼠时,它们表现出增加的进食习惯和减轻的焦虑感。抑制MC3R的化合物产生相反的效果-减少食物摄入量,但未观察到焦虑增加。
如果将这些结果转化为人类,该团队相信MC3R有潜力在一系列饮食和肥胖症的治疗中发挥作用。
该研究的主要作者范德比尔特大学医学院的神经科学家Michelle Bedenbaugh称:“这些结果中最令人兴奋的部分是,MC3R可能成为食欲失调(例如厌食症)以及肥胖症的潜在治疗靶标,如果我们能够实现从小鼠到人类的转变,那么这无疑将为人类提供帮助。”
研究人员强调,在开发有效疗法的漫长过程中,对模型生物体内药物靶标的识别是必不可少的早期步骤。
这项研究的资深作者,LSI主任兼UM医学院分子与整合生理学教授Roger Cone说:“这为我们提供了一种解决此电路的新方法,并明确了药物开发工作的重点。因此,这是开发药物的第一步,但显然很关键。”
事实上,MC3R电路从未像现在这样可视化,而且神经内分泌和行为电路的参与范围大大扩展了其对能量稳态的重要性。
原始出处:
The melanocortin-3 receptor is a pharmacological target for the regulation of anorexia.DOI: 10.1126/scitranslmed.abd6434
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#饮食失调#
59
#新途径#
50
新发现,但愿可以用于临床患者治疗
89
#肥胖症#
71
#SCIE#
50
非常好的文章
69
好文章!
88
好文章!
93
不错子,支持一下~
71