必看!2016年糖尿病相关研究亮点精华汇总
2016-12-14 MedSci MedSci原创
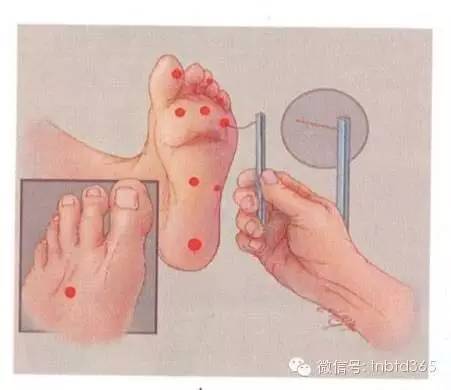
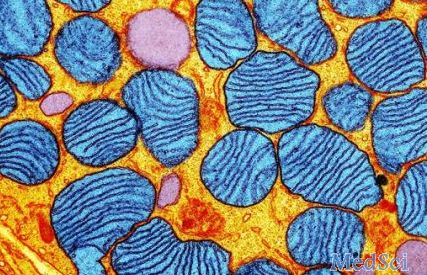
时光荏苒,岁月如梭,锦年素时,稍纵即逝,又是到年终盘点的时刻!相比于去年,2016年糖尿病取得了重大的研究成果,不论从基础还是临床研究,从不同方向、不同角度对糖尿病及其并发症的临床诊治进行了深入研究,为糖尿病的临床管理寻找最新方向。本文梅斯医学编辑就2016年糖尿病相关研究亮点进行汇总。【1】BMC Biotechnology:糖尿病福音,转基因蛆虫治疗足溃疡!北卡罗来纳州大学的研究人员发现,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关研究#
61
获益匪浅
102
感想,敢做,才能成功
0
再次学习并分享感谢
103
高大上的研究啊
98
字习了学习再次学习
111
跟进新进展
75
不错学习并分享感谢
53
思路很好
71
挺好的,学习了
51