Signal Transduct Target Ther.:治疗慢性疼痛的新发现
2021-06-06 Viho MedSci原创
阿片类药物仍然是治疗中度至严重急性疼痛的处方最广泛的止痛药之一,但它们的使用往往会导致呼吸抑郁、恶心和便秘,以及成瘾和耐受性,这些缺点大大减少了慢性和顽固性疼痛的治疗选择。

阿片类药物仍然是治疗中度至严重急性疼痛的处方最广泛的止痛药之一,但它们的使用往往会导致呼吸抑郁、恶心和便秘,以及成瘾和耐受性,这些缺点大大减少了慢性和顽固性疼痛的治疗选择。
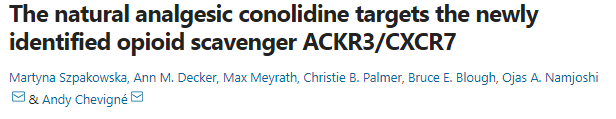
近日发表在国际期刊Signal Transduction and Targeted Therapy 上,科学家们在其先前研究结果的基础上,与非营利性研究机构RTI国际公司(RTI)的药物发现中心合作,证明了从风车花中提取的、传统上用于中医的天然止痛剂可乐定与新发现的阿片受体ACKR3/CXCR7相互作用,该受体调节大脑中自然产生的阿片肽。研究人员还开发了一种科诺立德的合成类似物RTI-5152-12,它在受体上显示出更大的活性。
阿片肽是一种小蛋白质,通过与大脑中的四个经典受体("分子开关")相互作用,介导疼痛缓解和情绪,包括欣快感、焦虑、压力和抑郁。免疫药理学和互动组学负责人Andy Chevigné博士和他的团队之前已经确定趋化因子受体ACKR3是一种新的第五种非典型阿片受体,对各种天然阿片具有高亲和力。ACKR3的功能是作为 "清道夫","捕获 "分泌的阿片类药物,防止它们与经典受体结合,从而抑制它们的镇痛活性,并作为阿片类药物系统的调节器。
植物历来是镇痛生物碱的来源,尽管它们的药理特性往往是有限的。在热带开花灌木的树皮中发现了这种天然的镇痛分子--可乐定。在目前的研究中,研究人员通过对240多个受体进行筛选,看它们是否有能力被这种分子激活或抑制,从而确定ACKR3是对具有镇痛特性的生物碱—可立定反应最强烈的靶点。
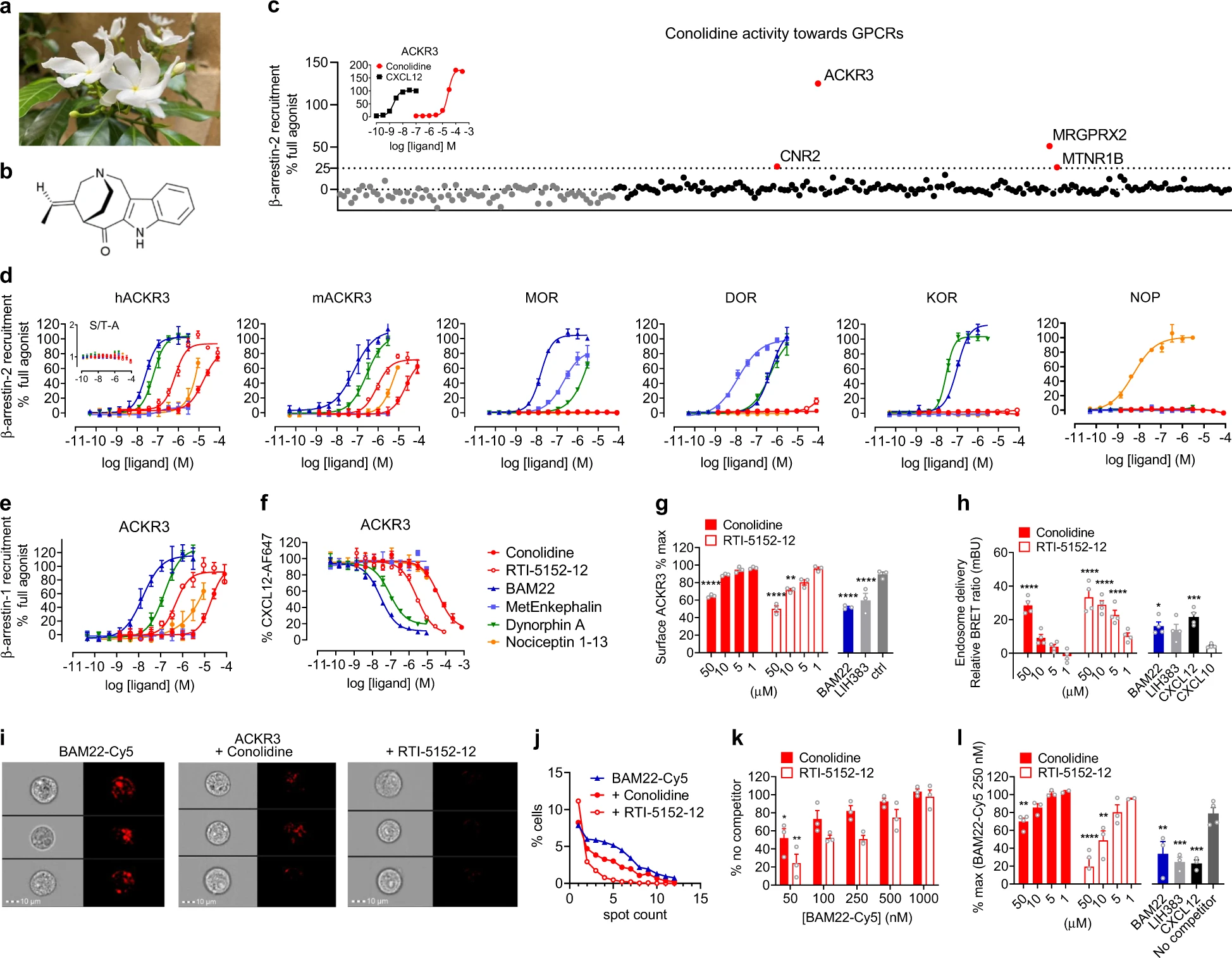
可乐定是阿片清除剂ACKR 3的激动剂
研究证实,可立定与新发现的阿片受体ACKR3结合,而对其他四个经典的阿片受体没有显示出亲和力。通过这样做,可乐定阻断了ACKR3,并阻止它捕获自然分泌的阿片类药物,这反过来又增加了它们与经典受体相互作用的可用性。研究人员相信,这种分子机制是这种传统药物对缓解疼痛的有益作用的基础。基因表达分析表明,ACKR 3在与重要阿片活性中心相对应的多个脑区高度表达。此外,它的表达水平往往高于经典阿片受体,这进一步支持了其在体外观察到的阿片肽清除能力的生理相关性。
可乐定的系统化学修饰导致了一种新化合物(RTI-5152-12),其对ACKR 3的作用提高了15倍。天然可乐定及其类似物均能以浓度依赖性的方式抑制ACKR 3对内源性阿片肽BAM 22的摄取,RTI-5152-12被认为能够增加与大脑中经典阿片受体结合的阿片肽的水平,从而提高止痛活性。
LIH免疫药理学和相互作用组组长Chevigné博士说:"发现ACKR3作为科诺立德的靶点,进一步强调了这种新发现的受体在调节阿片系统中的作用,从而调节了我们对疼痛的感知。
我们的研究结果还可能意味着,可立定,以及可能还有它的合成类似物,可能为治疗慢性疼痛和抑郁症带来新的希望,特别是考虑到可立定被报道引发较少的有害副作用--即成瘾性、耐受性和呼吸问题--与常用的阿片类药物如吗啡和芬太尼有关。"
因此,这些发现可以为开发一类具有替代作用机制的新药物奠定基础,从而有助于解决与阿片类药物滥用和成瘾日益严重有关的公共卫生危机,为ACKR 3与疼痛调节之间的相关性提供了进一步的证据,并开辟了治疗慢性疼痛的替代治疗途径。
文章参考:Martyna Szpakowska, Ann M. Decker, Max Meyrath, Christie B. Palmer, Bruce E. Blough, Ojas A. Namjoshi, Andy Chevign�. The natural analgesic conolidine targets the newly identified opioid scavenger ACKR3/CXCR7. Signal Transduction and Targeted Therapy, 2021; 6 (1) DOI: 10.1038/s41392-021-00548-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Signal#
83
#新发现#
72
#target#
91
#TRA#
91
#Sign#
93
#慢性疼痛#
90
好的开头,期待进展!
91
赚点积分
106