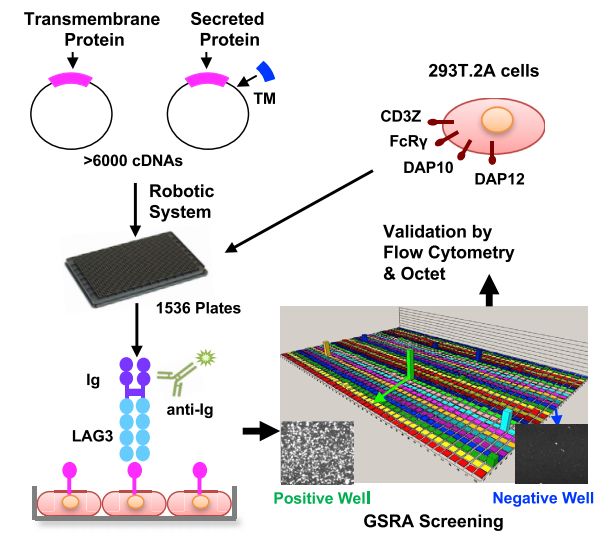
Nature:破解免疫治疗耐药性!哈佛科学家找到了肿瘤对免疫检查点抑制剂耐药的关键基因,免疫治疗疗效有望全面提升
2018-12-31 奇点糕 奇点网
当下免疫治疗热,越来越多的企业参与到免疫治疗药物的研发中,截止目前我国已经有4款免疫检查点抑制剂获批治疗癌症。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#抑制剂#
61
#Nat#
62
#关键基因#
89
学习学习谢谢
112
#免疫检查点#
80
#哈佛#
75
谢谢梅斯提供这么好的信息,学到很多
81