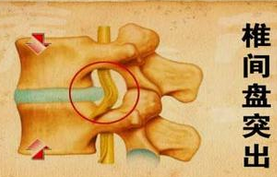
腰椎间盘突出 如何绕开诊治误区
2018-04-13 张俊,衣晓峰 健康报医生频道
患了腰椎间盘突出症,几乎所有的大夫都会告诉病人,练“小燕飞”,可是有的腰椎间盘突出的病人,“小燕飞”可以做200次了,可病还是不好;对腰椎间盘突出的人,医生常常建议睡硬板床,可睡了硬板床以后,腰痛好像更重了;因腰部不适去医院看病后,拍片显示有腰椎骨质增生,做了手术后,但病情仍没有任何缓解。诸如此类的困惑,在腰椎间盘突出的临床中司空见惯。那么,这些问题应该如何认识,又该怎样解释呢?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













很赞
122
#椎间盘突出#
85
#腰椎#
91
#误区#
86
#腰椎间盘#
80
现代病很多.要认真研读
105
学习了.谢谢分享.
106