Blood:靶向抑制CD47-SIRPα的治疗活性需要Fc-FcγR的相互作用
2019-08-07 MedSci MedSci原创
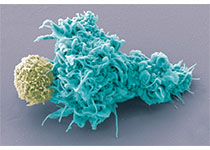
CD47抗体,与肿瘤细胞上的CD47结合、阻断其与吞噬细胞上的SIRPα相互作用,在多种癌症中均具有抗肿瘤作用,包括T细胞淋巴瘤(TCL)。近期,研究人员发现细胞表面的CD47在原发性TCLs上的差异性表达,而也可以抑制吞噬作用的I型MHC普遍表达。多种单克隆抗体(mAbs)可阻断CD47-SIRPα相互作用,促进TCL细胞的吞噬作用,靶向I型MHC的抗体一起应用时可增强该作用。在TCL系中,表面
多种单克隆抗体(mAbs)可阻断CD47-SIRPα相互作用,促进TCL细胞的吞噬作用,靶向I型MHC的抗体一起应用时可增强该作用。在TCL系中,表面CD47和调节CD47凝集的基因的表达水平与CD47阻断诱导的吞噬作用程度无关。
用CD47单抗短疗程治疗多发性人TCL患者来源的移植瘤(PDXs)或具有免疫功能的小鼠TCL模型,可显著降低其淋巴瘤负担,延长存活期。耗竭体内的吞噬细胞可拮抗CD47抗体的作用,但耗竭中性粒细胞无此效应。
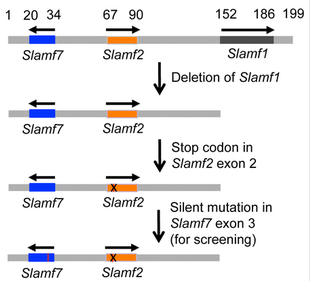
仅抗CD47抗体的F(ab’)2片段不能诱导人巨噬细胞的吞噬作用,提示该过程需要Fc-FcγR相互作用。相反,仅F(ab’)2片段可增强小鼠巨噬细胞的吞噬作用,且与SLAMF7-Mac-1互用无关。全长的抗CD47 mAb也可诱导FcγR缺陷小鼠巨噬细胞的吞噬作用。与抗CCR4 mAb、mogamulizumab或I型MHC封闭抗体一起应用时可放大IgG1抗CD47mAb诱导吞噬作用和NK细胞介导的TCL细胞毒性。
本研究结果有助于解释与患者相比,在小鼠模型中使用阻断CD47的药物具有不同的治疗活性,还对单独或联合应用抗CD47单克隆抗体具有指导意义。
Salvia Jain, et al.Targeted Inhibition of CD47-SIRPα Requires Fc-FcγR Interactions to Maximize Activity in T-cell Lymphomas. Blood 2019 :blood.2019001744; doi: https://doi.org/10.1182/blood.2019001744
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CD4#
33
#相互作用#
40
#SIrP#
50
#CD47-SIRPα#
58
#互作#
36