Eur J Neurol.:视觉空间功能障碍与非痴呆性脑淀粉样血管病中白质损害的后部分布相关
2021-06-27 MedSci原创 MedSci原创
非痴呆性CAA患者存在视觉空间功能障碍,尤其是视觉物体感知障碍,且与脑白质损伤的后向倾向独立相关,而与SVD影像学标志物的整体严重程度或出血标志物的分布模式无关。这一发现提示后部白质的损害而不是整体
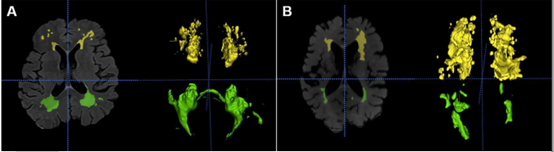
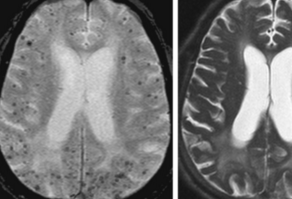
脑淀粉样血管病(CAA)的病理特征是β-淀粉样蛋白(Aβ)在皮质和软脑膜的小动脉沉积,这是最常见和严重的后部脑区。大量研究表明,CAA是公认的老年人血管性认知损害和阿尔茨海默病痴呆的决定因素,依赖或独立于脑出血(ICH)事件。CAA患者在几个神经心理学领域表现较差,特别是执行功能和情景记忆。由于大脑后部病变可导致视空间功能障碍,如后部皮质萎缩中突出的视觉处理缺],一些小队列研究表明CAA患者存在视空间损害。视觉物体和空间知觉(VOSP)测试特别适合于中风后偏瘫患者,无需书写或绘画,可分为针对视觉知觉不同成分的子测试。 Su Y等假设非痴呆的CAA患者存在VOSP测量的视空间功能障碍,这可能与缺血和/或出血的SVD成像标记物的严重程度或分布有关。该研究成果发表在 Eur J Neurol杂志。 该研究的目的是探讨CAA的视觉空间功能障碍是否与小血管疾病(SVD)影像学标志物的后部分布有关。 研究流程图 从中国前瞻性队列中招募60例非痴呆CAA患者,30例非CAA SVD患者作为对照。使用视觉对象和空间知觉(VOSP)测试来评估视觉空间能力,并使用多变量回归模型来评估它们与奇异值
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#脑淀粉样#
82
#视觉空间#
69
#白质#
114
#血管病#
104
#Neurol#
64
#功能障碍#
62
#视觉#
89
#脑淀粉样血管病#
116
老年人痴呆何药可用??
79