Diabetologia:脂质环境诱导2型糖尿病患者免疫细胞的ER应激,TXNIP表达及炎症反应
2018-04-24 MedSci MedSci原创
近日,国际杂志 《Diabetologia》上在线发表一项关于脂质环境诱导2型糖尿病患者免疫细胞的ER应激,TXNIP表达和炎症反应的研究。 肥胖和2型糖尿病会与影响胰岛素敏感性和胰岛素分泌的低度炎症同时发生。最近研究表明含有3(NLRP3)炎性蛋白的pyrin结构域的硫氧环相互作用蛋白(TXNIP)参与NOD样受体家族激活过程。在这项研究中,研究人员旨在确定TXNIP的表达是否在2型和1型
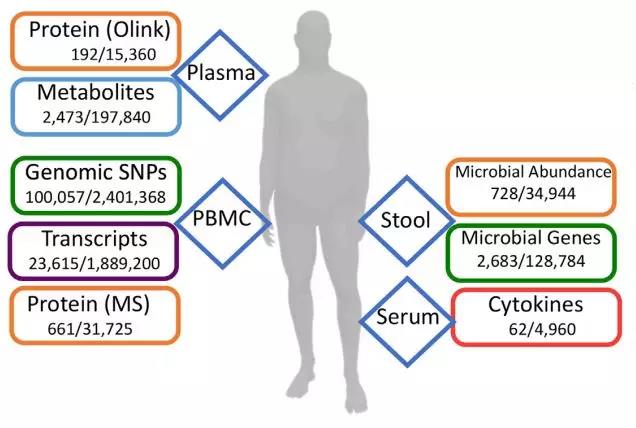
近日,国际杂志 《Diabetologia》上在线发表一项关于脂质环境诱导2型糖尿病患者免疫细胞的ER应激,TXNIP表达和炎症反应的研究。 肥胖和2型糖尿病会与影响胰岛素敏感性和胰岛素分泌的低度炎症同时发生。最近研究表明含有3(NLRP3)炎性蛋白的pyrin结构域的硫氧环相互作用蛋白(TXNIP)参与NOD样受体家族激活过程。在这项研究中,研究人员旨在确定TXNIP的表达是否在2型和1型糖尿病患者的循环免疫细胞中发生改变,以及是否这与炎症的具体发生原因和后果有关。 研究人员通过实时定量PCR(qRT-PCR)对13例非糖尿病个体,23例1型糖尿病患者和81例2型糖尿病患者的外周血单核细胞(PBMC)中TXNIP,炎症标志物,未折叠蛋白应答(UPR)对内质网(ER)应激的标记和参与鞘脂代谢的酶的表达进行定量。对13名非糖尿病个体,35名1型糖尿病患者和94名2型糖尿病患者的血浆进行脂质组学分析。在人类单核细胞衍生的巨噬细胞(HMDMs)和THP-1细胞中分析ER应激或特定脂质对TXNIP和炎症标记物表达的影响。 研究发现,与非糖尿病个体或1型糖尿病个体相比,2型糖尿病患者的PBMC中
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
68
#BET#
62
#炎症反应#
65
#2型糖尿病患者#
65
#应激#
52
#糖尿病患者#
63
#ER应激#
74