JOT:踝关节骨折围手术期评价只看X线不靠谱
2022-08-27 放射沙龙 MedSci
通过考察踝关节骨折切开复位内固定术术中透视和术后平片的灵敏度、特异度、观察者间信度和观察者内信度等指标评价术后的关节对合程度。
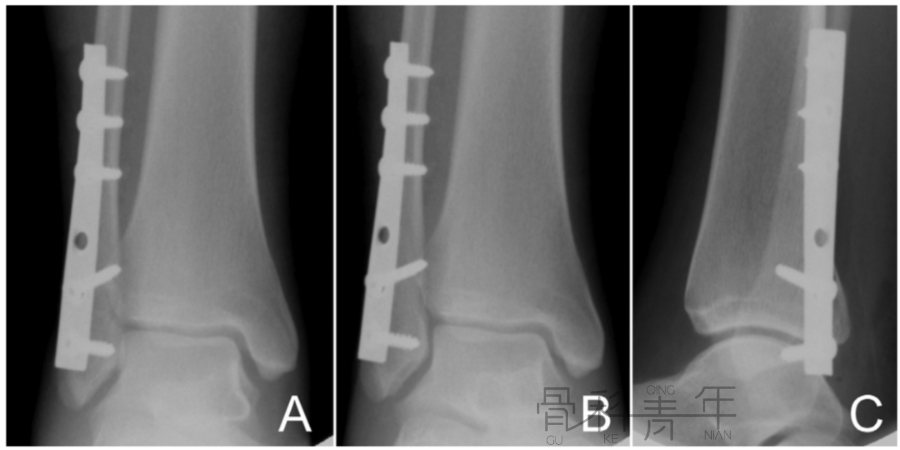
踝关节骨折往往会导致创伤性关节炎,其中一个重要的原因就是骨折引起关节脱位进而改变了关节正常的力学关系,所以对于骨科医生,能否使踝关节恢复解剖复位对于术后恢复情况的评价至关重要。来自纽约的Matthew R. Garner医生等人发现,在进行踝关节骨折的切开复位内固定术时,仅仅依靠围手术期的透视和X线片结果来评价关节的复位情况并不能达到理想效果,并将其研究结果发表在近期的J Orthop Trauma上,现介绍如下。
目的:
通过考察踝关节骨折切开复位内固定术术中透视和术后平片的灵敏度、特异度、观察者间信度和观察者内信度等指标评价术后的关节对合程度。
方法:
本研究回顾性分析了105例踝关节骨折术后病人,所有患者均行切开复位内固定术。考察术中透视和X线平片与CT图像比较之下,其对于踝关节对合程度判断能力的灵敏度、特异度、观察者间信度和观察者内信度,进而评价常规围手术期影像学资料的可信程度。
结果 术中透视和X线片的灵敏度分别是21%和36%。特异度分别是95%和89%。术中透视的观察者间信度是K= 0.15,平均观察者内信度为K = 0.32。X线片的平均观察者内信度为K= 0.30和K = 0.59。
 结论:
结论:
尽管结果显示术中透视和术后X线片的特异度可以接受,然而在评价踝关节对合度时两者的信度和灵敏度都较低。此结果填补了目前文献中关于关节复位切开复位内固定术围手术期常规影像学检查准确程度的空白。在此结论基础上,可以认为:在进行踝关节骨折的切开复位内固定术中,即使透视显示骨折部位已经达到解剖复位,术者亦应对此结果保持怀疑,并且在可能的情况下,尽量通过直视关节面来确认复位情况。另外,对于病情严重,提示可能临床结局不良的患者,即使通过常规影像学检查“看起来”已经达到了关节的解剖复位,术后也应当拍摄轴位片以防隐蔽的关节对位不良。对于有条件的医疗机构,可以在术中使用CT检查,使术者充分掌握实时的关节情况。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#手术期#
119
#靠谱#
73
#X线#
110
#踝关节骨折#
117
#评价#
77
#踝关节#
78