JAHA:替卡格雷与氯吡格雷对冠状动脉疾病患者心肌灌注的疗效比较!
2017-05-08 xing.T MedSci原创
由此可见,替卡格雷可以增强稳定的冠状动脉疾病患者整体和区域腺苷诱导的MBF。这种效应可能有助于获得改善死亡的好处,相比于氯吡格雷治疗。
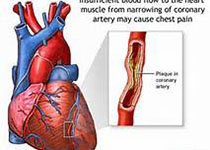
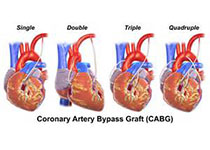
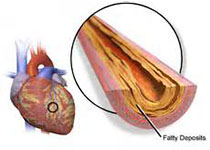
替卡格雷是一种血小板P2Y12受体抑制剂,可用于急性冠状动脉综合征患者,以降低血小板活性和减少血栓形成。替卡格雷与在氯吡格雷中观察到的死亡增量减少相关,这可能与其非抗血小板作用相关。动物模型的证据表明替卡格雷可以增强腺苷诱导的心肌血流量(MBF)。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员比较了采用替卡格雷与氯吡格雷治疗的稳定性冠状动脉疾病患者休息时和腺苷诱导充血是的MBF。
在这项随机双盲交叉研究中,研究人员纳入了22例患者,分别接受每天两次口服90mg替卡格雷10天或每天一次口服氯吡格雷75mg治疗,在不同治疗之间至少冲洗10天。研究人员采用铷82正电子发射断层扫描/计算机断层扫描测量了休息、中间剂量和高剂量腺苷后诱导的整体和区域MBF和心肌血流储备。
研究人员发现采用替卡格雷治疗相比于氯吡格雷治疗的中间剂量的腺苷诱导的整体MBF明显更大(1.28±0.55 vs. 1.13±0.47毫升/分钟每克,P=0.002),而基础(0.65±0.19 vs. 0.60±0.15毫升/分钟每克,P=0.084)和高剂量腺苷(1.64±0.40 vs. 1.61±0.19毫升/分钟每克,P=0.53)诱导无明显差异。在心肌血流储备受损(<2.5)的区域,中、高剂量的腺苷诱导的区域MBF在替卡格雷治疗组明显要比氯吡格雷治疗更大(P<0.0001),但基础差异没有显著性。
由此可见,替卡格雷可以增强稳定的冠状动脉疾病患者整体和区域腺苷诱导的MBF。这种效应可能有助于获得改善死亡的好处,相比于氯吡格雷治疗。
原始出处:
Matthieu Pelletier‐Galarneau, et al. Randomized Trial Comparing the Effects of Ticagrelor Versus Clopidogrel on Myocardial Perfusion in Patients With Coronary Artery Disease.JAHA.2017. https://doi.org/10.1161/JAHA.117.005894
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疾病患者#
74
#心肌灌注#
75
#冠状动脉疾病#
103
#AHA#
77
#替卡格雷#
86