Haematologica:Isatuximab 加卡非佐米和地塞米松与卡非佐米和地塞米松在肾功能不全的复发性多发性骨髓瘤患者中的比较
2021-12-21 MedSci原创 MedSci原创
在 肾损害(RI) 患者中,将伊萨妥昔单抗 (Isa)添加到地塞米松 (Kd) 中改善了临床结果,并具有可控的安全性,这与在整体 IKEMA 研究人群中观察到的益处一致。
多发性骨髓瘤(MM)的特征是浆细胞的异常增殖和m蛋白,一种单克隆免疫球蛋白(Ig)的产生。肾损伤(RI)影响多达50%的MM患者。mm相关的RI是多因素的,但主要是由于远端小管中无igg轻链的沉淀,导致小管梗阻和铸造性肾病。肾损害 (RI) 在多发性骨髓瘤 (MM) 患者中很常见,因此需要可以改善肾功能的新疗法。
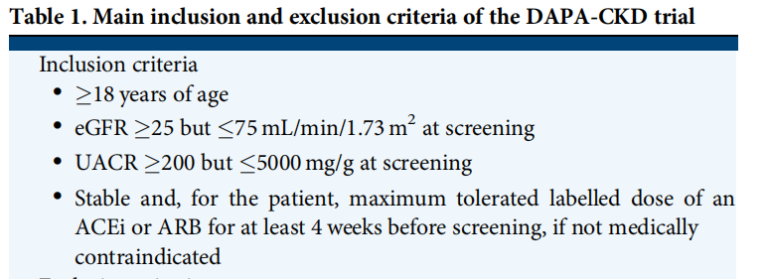
IKEMA(NCT03275285)是一项前瞻性、多国、随机、开放标签、平行组的3期研究,在16个国家的69个研究中心进行,研究了伊萨妥昔单抗 (Isa) 与卡非佐米和地塞米松 (Kd) 在复发性 MM 中与 Kd 的比较。该亚组分析检查了 RI 患者的结果,RI 定义为估计肾小球滤过率 <60 mL/min/1.73 m²。
该研究方法的细节以前已经报道过。简单地说,符合条件的患者复发了MM,既往有1-3种治疗方法。如果患者有原发性难治性MM或仅血清游离轻链可测量疾病,既往接受过卡非佐米治疗,抗cd38抗体治疗难治,或左心室射血分数<40%,则排除。基线估计的肾小球滤过率(eGFR)低至15个mL/min/1.73m²的患者有资格进行登记。30例既往有肺共病的患者,包括慢性阻塞性肺疾病,可纳入研究。


图1:Isa-Kd与Kd相比的无进展生存期。(A)RI患者(eGFR<60mL/min/1.73m²)或无RI的(B)患者(eGFR≥60mL/min/1.73m²),(ITT人群)。PFS根据盲法独立反应委员会。 d: 地塞米松、eGFR:估计肾小球滤过率、Isa:伊沙妥昔单抗、ITT:有治疗意图、K:卡非佐米、PFS:无进展生存期。
Isa-Kd组患者在第一个28天周期的第1、8、15和22天静脉注射10mg/kg静脉注射;随后的周期的第1天和第15天。在两组中,卡非佐米在第1和第2天静脉注射20mg/m2;在第1周期的第8、9、15和16天注射56mg/m2;然后在后续周期的第1、2、8、9、15和16天给予56mg/m2。28地塞米松在第1、2、8、9、15、15、16、22、23天静脉或口服20mg。继续治疗至不可接受的不良事件(AE)、疾病进展或其他停药标准。
研究终点和测量结果主要疗效终点为PFS,关键的次要疗效终点包括根据国际骨髓瘤工作组(IMWG)缓解标准的总缓解率(ORR)、31个非常好的部分缓解(VGPR)或更好的缓解率、可测量的残留疾病(MRD)阴性率、完全缓解(CR)率和OS。
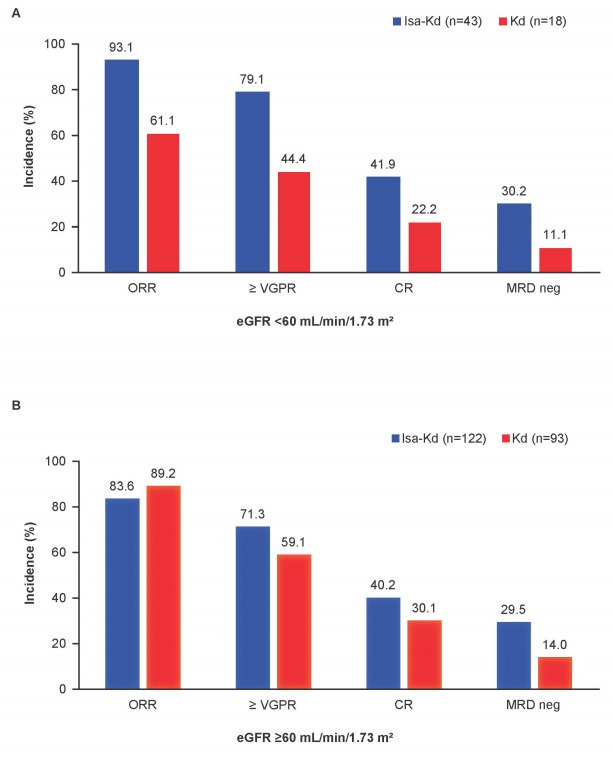
图2:对Isa-Kd与Kd的应答率进行了比较。(A)患者伴有RI(eGFR<60mL/min/1.73m²)或无RI的(B)患者(eGFR≥60mL/min/1.73m²),(ITT人群)。CR:完全反应;d:地塞米松;eGFR:估计肾小球滤过率;Isa:伊沙妥昔单抗;ITT:意图治疗;K:卡非佐米;MRD阴性:微小残留疾病阴性;ORR:总体反应率;PR:部分反应;VGPR:非常好的部分反应。MRD通过下一代测序进行评估,敏感性水平为10-5。
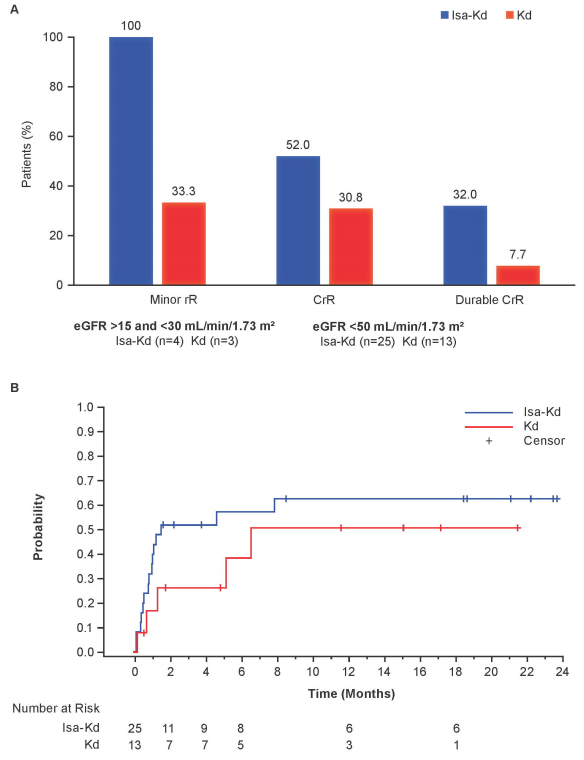
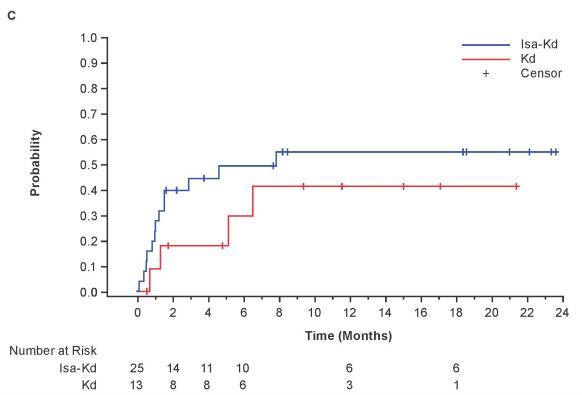
图3:Isa-Kd和Kd臂的肾脏反应。(A)基线eGFR<50mL/min/1.73m²患者完全和持久(≥60天)肾脏反应,基线eGFR≥15和<30mL/min/1.73m²患者轻微肾脏反应(ITT人群)。(B)基线时eGFR<50mL/min/1.73m²患者首次完成肾反应的时间和首次完成肾反应的(C)时间。CrR:完全肾反应d:地塞米松eGFR:估计肾小球滤过率Isa:伊沙妥昔单抗ITT:治疗意图K:卡非佐米rR:肾脏反应。
结果显示,添加 Isa 延长了 RI 患者的 PFS(风险比,0.27;95% CI,0.11-0.66;Isa-Kd 的中位 PFS 未达到,而 Kd 的中位 PFS 为 13.4 个月 [20.8 个月随访])。Isa-Kd (52.0%) 和 Kd (30.8%) 的完全肾脏反应发生率更高,并且分别在 32.0% 和 7.7% 的患者中持久。Isa-Kd 的治疗暴露时间更长,开始周期的中位数和暴露持续时间的中位数分别为 20 对 9 周期和 81.0 对 35。Isa-Kd 与 Kd 分别为 7 周。在 RI 患者中,两组之间发生≥3 级治疗出现不良事件的患者发生率相似(Isa-Kd 为 79.1%,Kd 为 77.8%)。
总之,研究表明,在 RI 患者中,将 Isa 添加到 Kd 改善了临床结果,并具有可控的安全性,这与在整体 IKEMA 研究人群中观察到的益处一致。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#复发性#
115
#肾功能#
79
#复发性多发性骨髓瘤#
81
#多发性#
74
#HAE#
64
#mAb#
61
👍
92
#肾功能不全#
87
#EMA#
68
#isatuximab#
68