Nature review immunology:胆固醇炎症反应与动脉粥样硬化
2015-01-27 佚名 生物谷
进入工业化社会以来,人们的饮食发生了很大的改变。长期食用富含脂肪与固醇的食物使血液系统中富含胆固醇的低密度脂蛋白(LDL)含量增高,促进了胆固醇在动脉血管壁上的过量沉积,并且引起炎症反应,最终造成动脉粥样硬化。修饰后LDL作为一类细胞表面TLR的配体,本身可以触发先天性免疫反应,巨噬细胞受到修饰后LDL的刺激后会发生吞噬作用,从而造成了胆固醇在胞内的累积,而这一效应又会增强下一轮的免疫反应。另一方
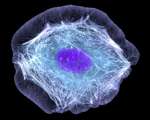
进入工业化社会以来,人们的饮食发生了很大的改变。长期食用富含脂肪与固醇的食物使血液系统中富含胆固醇的低密度脂蛋白(LDL)含量增高,促进了胆固醇在动脉血管壁上的过量沉积,并且引起炎症反应,最终造成动脉粥样硬化。修饰后LDL作为一类细胞表面TLR的配体,本身可以触发先天性免疫反应,巨噬细胞受到修饰后LDL的刺激后会发生吞噬作用,从而造成了胆固醇在胞内的累积,而这一效应又会增强下一轮的免疫反应。另一方面,高密度脂蛋白(HDL)能够将胆固醇从胞浆内向外运输,这一过程会起到控制免疫反应的效果。以上说明胆固醇在胞浆内的积累能够调控免疫反应。然而这一过程是如何发生的呢?
原始出处
Tall AR1, Yvan-Charvet L2.Cholesterol, inflammation and innate immunity.Nat Rev Immunol. 2015 Jan 23
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









前因后果,还是互为因果,还是缠绵不休!
152
#Nat#
61
#review#
0
#粥样硬化#
67
已阅
182
#炎症反应#
65