Oncotarget:抗β2微球蛋白单克隆抗体能改善硼替佐米的耐药性
2015-05-08 沐晴 译 MedSci原创
硼替佐米(BTZ)是目前用于治疗多发性骨髓瘤和套细胞淋巴瘤的一种蛋白酶抑制剂,因其存在许多副作用及耐药性,硼替佐米在临床的广泛应用受到限制。研究认为,细胞存活和死亡受到细胞凋亡和自噬活动的交叉调节,而且,自噬可以通过抑制半胱天冬酶的清除抑制细胞凋亡。近来研究发现,自噬在调节化疗药物耐量性中起很重要的作用,BTZ可以激活肿瘤细胞的自噬。BTZ诱导的细胞自噬对于BTZ耐药的乳腺癌细胞非常重要,提示抑制
硼替佐米(BTZ)是目前用于治疗多发性骨髓瘤和套细胞淋巴瘤的一种蛋白酶抑制剂,因其存在许多副作用及耐药性,硼替佐米在临床的广泛应用受到限制。研究认为,细胞存活和死亡受到细胞凋亡和自噬活动的交叉调节,而且,自噬可以通过抑制半胱天冬酶的清除抑制细胞凋亡。近来研究发现,自噬在调节化疗药物耐量性中起很重要的作用,BTZ可以激活肿瘤细胞的自噬。BTZ诱导的细胞自噬对于BTZ耐药的乳腺癌细胞非常重要,提示抑制肿瘤细胞的自噬或许能改善BTZ的耐药。

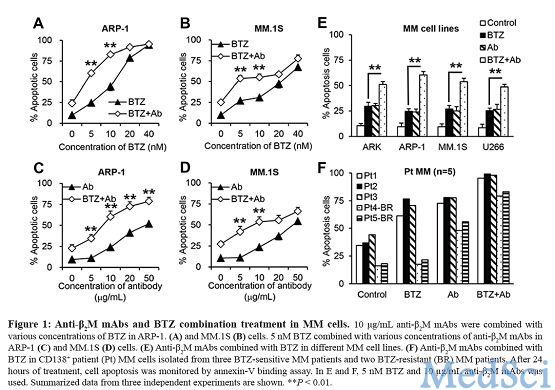
研究者对自噬基因beclin 1启动子区进行序列分析,结果推定,从第615 到789 bp,有3个NF-κB结合位点。然而在MM细胞中,联合抗-β2M mAbs治疗时,BTZ可以增加NF-κB的转录活性,而且,联合治疗可以抑制NF-κB p65与beclin 1 启动子结合。此外,在小鼠MM模型中,抗-β2M mAbs和BTZ联合治疗可以抑制MM细胞的活性。因此,这篇研究为抗-β2M mAbs和BTZ联合治疗走向临床提供了证据支持,有助于克服BTZ的药物抵抗,从而提高MM病人的存活率。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#体能#
65
#克隆#
76
#target#
64
#球蛋白#
0
看看
161