Hypertension:蛋白尿可作为肾动脉支架治疗的判断指标
2016-09-22 MedSci MedSci原创
这些数据表明,低蛋白尿的肾动脉狭窄患者才是肾动脉支架置入术加优化药物治疗,获得临床益处潜在的治疗对象,但是需要进一步的研究来证实这些初步的观察。
在肾动脉粥样硬化病变与心血管结局的随机临床试验中,研究者并没有发现肾动脉支架放置比最佳的药物治疗方案有额外的临床益处。然而,肾动脉支架植入的研究未对蛋白尿与治疗预后的关系进行评估。近日高血压领域权威杂志《Hypertension》发表了加拿大多伦多Sheldon
Tobe教授及其团队有关肾动脉粥样硬化性狭窄患者肾动脉支架治疗与蛋白尿关系的研究。
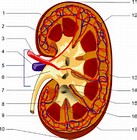
研究通过对肾动脉粥样硬化病变与心血管结局的随机临床试验的数据进行深入挖掘,根据研究人群的中位基线尿白蛋白/肌酐比值将826名研究对象分为两组,同时分析主要指标的5年发病率(这些指标包括:心肌梗死、充血性心脏衰竭、中风、肾脏替代治疗、进行性肾功能不全、或心血管疾病或肾脏疾病相关的死亡),以及主要指标中每个疾病的生存率和总生存率。
这些数据表明,低蛋白尿的肾动脉狭窄患者才是肾动脉支架置入术加优化药物治疗,获得临床益处潜在的治疗对象,但是需要进一步的研究来证实这些初步的观察。
原始出处:
Timothy P. Murphy,et al. Relationship of Albuminuria and Renal Artery Stent Outcomes Results From the CORAL Randomized Clinical Trial (Cardiovascular Outcomes With Renal Artery Lesions). Hypertension. 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
88
#肾动脉#
83
#支架治疗#
66
#TENS#
64
#肾动脉支架#
91
对我很有帮助,感谢。
86
对我很有帮助,感谢。
99
#Hypertension#
55