IBD:患有艰难梭菌感染的炎性肠病患者出院后 90天内再入院的危险因素分析
2021-03-28 MedSci原创 MedSci原创
艰难梭菌感染(CDI)被认为是一种公共卫生问题,它会导致患者住院时间,费用,死亡率和结肠切除率增加,特别是对于炎症性肠病患者来说,这样的影响更为明显。
艰难梭菌感染(CDI)被认为是一种公共卫生问题,它会导致患者住院时间,费用,死亡率和结肠切除率增加,特别是对于炎症性肠病患者来说,这样的影响更为明显。美国有300万人患有炎症性肠病(IBD),IBD和艰难梭菌之间的关联尚不清楚,但是有研究显示炎症性肠病(IBD)患者的艰难梭菌感染(CDI)风险增加,且发病率和死亡率显着高于无IBD的患者。因此,本项研究旨在探究IBD患者住院后90天内特定疾病的再入院率和CDI感染的独立危险因素。

本项研究共收集了50799例因IBD急性发作的患者出院后再入院的临床数据。主要观察结局是患者出院后90天内因CDI感染再入院的情况,以及患者医疗支出情况。使用Cox回归分析确定再次入院的危险因素。

本项研究发现所有患者中90天的特定再入院率为0.1%(n = 477)。再入院时间总共有3,005天,再次入院的危险因素是机械通气> 24小时([HR],6.62,95%[CI],0.80-54.57);先前CDI感染的病史(HR,5.48; 95%CI,3.66-8.19); HIV阳性(HR,4.60; 95%CI,1.03-20.50); 酗酒(HR,2.06; 95%CI,1.15-3.70); 帕金森氏病(HR,4.68; 95%CI,1.65-13.31);复杂性溃疡性结肠炎(HR,4.49; 95%CI,2.80-7.18)。
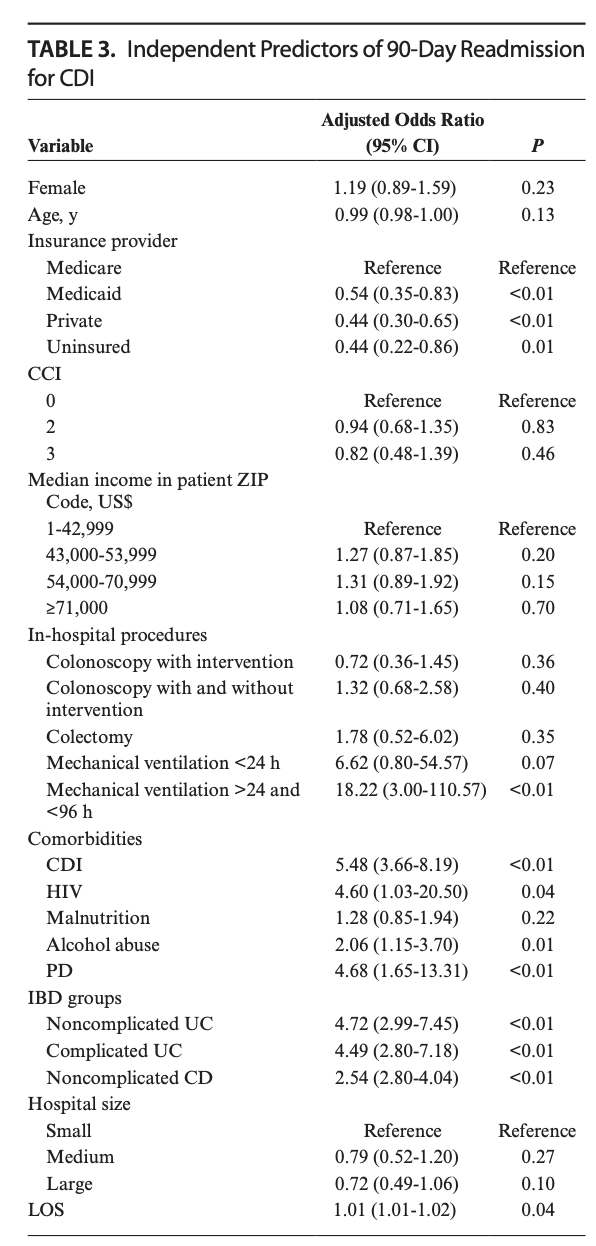
本项研究证实IBD复发后因CDI感染再入院的发生率为0.1%。同时研究人员也发现了与CDI相关的再次入院的风险因素,例如帕金森病的病史,既往的CDI感染史,HIV阳性状态和酗酒史。
原始出处:
Pedro Palacios Argueta. Et al. 90-Day Specific Readmission for Clostridium difficile Infection After Hospitalization With an Inflammatory Bowel Disease Flare: Outcomes and Risk Factors.Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#IBD#
63
受益匪浅
102
学到很多东西,谢谢平台
140
学习啦
137
有用知识。
121
学到了很多东西谢谢老师
138