Oncogenesis:ZFHX3对ERβ抑制细胞增殖是必不可少的
2019-04-28 AlexYang MedSci原创
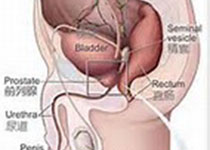
雌激素受体2(ESR2,也称之为ERβ)和锌指同源框3(ZFHX3,也称之为ATBF1)在小鼠中能够调控前列腺发育和抑制前列腺肿瘤的形成。ZFHX3对ESR1的功能是不可或缺的,ESR1与ESR2属于同一家族蛋白,但是在前列腺上皮中几乎不表达。ZFHX3怎样抑制前列腺致瘤过程仍旧不清楚。最近,有研究人员调查了是否ZFHX3和ERβ在抑制前列腺致瘤过程中存在互作。在C4-2B和LNCaP雄激素受体(
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Gene#
33
#细胞增殖#
42
#Oncogene#
52
#ESI#
44
很好的机制解析,感谢分享!
67