Blood:诱导Bruton酪氨酸激酶降解或许可成为癌症的新治疗策略
2019-01-06 MedSci MedSci原创
中心点:在癌细胞中,小分子诱导的BTK降解比单纯抑制BTK具有更好的抗增殖作用。在PDX淋巴瘤模型中,先导降解剂DD-03-171可降低肿瘤负担并延长模型动物的存活期。摘要:Bruton酪氨酸激酶(BTK)供价抑制剂依鲁替尼对多种B细胞恶性肿瘤都具有很高的抗癌效果。但,依鲁替尼对BTK没有选择性,存在多重耐药机制,如C481S-BTK突变,可使其疗效大打折扣。Dennis Dobrovolsky等
在癌细胞中,小分子诱导的BTK降解比单纯抑制BTK具有更好的抗增殖作用。
在PDX淋巴瘤模型中,先导降解剂DD-03-171可降低肿瘤负担并延长模型动物的存活期。
摘要:
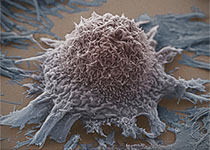
Bruton酪氨酸激酶(BTK)供价抑制剂依鲁替尼对多种B细胞恶性肿瘤都具有很高的抗癌效果。但,依鲁替尼对BTK没有选择性,存在多重耐药机制,如C481S-BTK突变,可使其疗效大打折扣。
Dennis Dobrovolsky等人假设用小分子诱导BTK降解或许可以克服传统酶抑制剂的一些局限性。现其证实BTK降解可有效抑制癌细胞的信号转导和增殖,而且BTK降解剂可有效降解C481S-BTK。
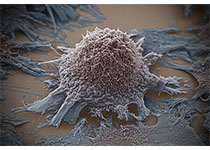
此外,研究人员还发现DD-03-171,一种经过优化的先导化合物,在体外时,可通过降解BTK、IKFZ1和IKFZ3来增强对套细胞淋巴瘤(MCL)细胞的抗增殖效应,而在体内时,对患者来源的移植瘤同样有效。
因此,“三重降解”可能是治疗MCL和克服依鲁替尼耐药的新方法,从而满足MCL和其他B细胞淋巴瘤治疗过程中未满足的一些主要需求。
Dennis Dobrovolsky,et al. Bruton's Tyrosine Kinase degradation as a therapeutic strategy for cancer. Blood 2018 :blood-2018-07-862953; doi: https://doi.org/10.1182/blood-2018-07-862953
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#酪氨酸激酶#
56
#激酶#
59
好
93
谢谢分享,学习了
96
了解一下,谢谢分享!
101