Eur Urol Focus:机器人部分肾切除术中的超选择性缺血并不能提供比肾动脉夹闭更好的长期肾功能结果
2021-05-09 AlexYang MedSci原创
肿瘤靶向动脉的超选择性夹闭旨在消除剩余肾脏的缺血,同时在切除过程中保持瘤床无血。
肿瘤靶向动脉的超选择性夹闭旨在消除剩余肾脏的缺血,同时在切除过程中保持瘤床无血。

最近,有研究人员评估了超选择夹闭对长期肾功能的影响,并与肾动脉早期脱夹进行了比较。
研究人员在2018年2月至2019年8月进行了一项随机的单中心单盲试验(1:1)。研究结果发现,6个月后,术后肾脏的相对评估的肾小球滤过率(eGFR)下降没有明显的差异(-21.4% vs -23.4%,p=0.66)。在对保留的肾脏体积百分比进行调整后,仍旧没有差异,而保留的肾脏体积是功能保存的一个独立的预测性因素。另外,在失血量、血红蛋白变化、术后并发症、输血以及转为根治性肾切除术(2例 vs. 0例)或转为开放手术(1例 vs. 0例)方面也没有明显差异。尽管效果良好,但鉴于没有有利于SS-RAPN的趋势,指导委员会在中期分析后以无效为由中断了该试验。
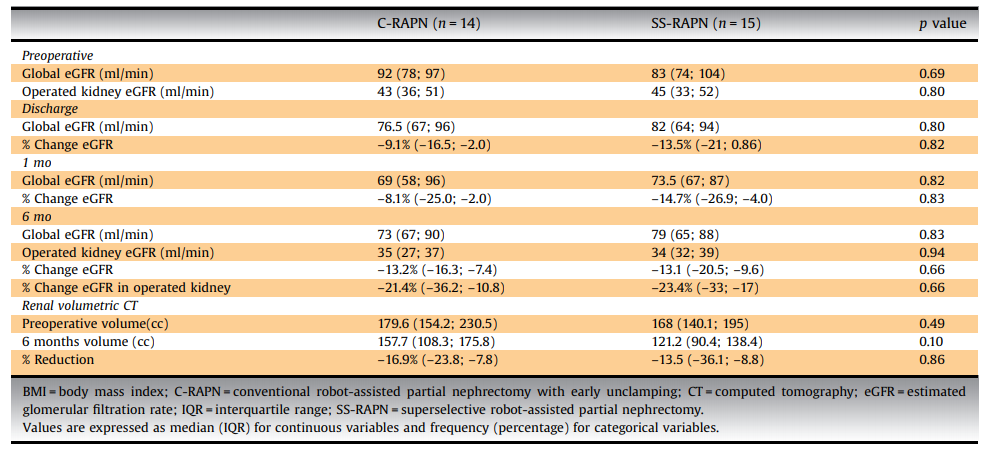
功能结果
最后,研究人员指出,使用近红外荧光色谱(NIRF)的超选择机器人辅助部分肾切除术(SS-RAPN)并不能提供比肾动脉夹闭更好的肾功能保留,但研究人员质疑这种技术在较高出血风险下的收益。
原始出处:
Jean-Alexandre Long, Gaëlle Fiard, Joris Giai et al. Superselective Ischemia in Robotic Partial Nephrectomy Does Not Provide Better Long-term Renal Function than Renal Artery Clamping in a Randomized Controlled Trial (EMERALD): Should We Take the Risk? Eur Urol Focus. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肾功能#
64
#肾切除术#
73
#肾动脉#
97
#切除术#
61
#选择性#
115
#机器人#
86
#机器#
53