PNAS:抗真菌感染新策略:首次发现雷帕霉素靶蛋白TOR感知磷酸
2017-06-01 BioArt BioArt
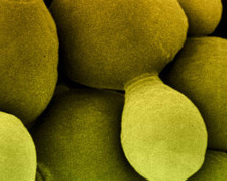
编者按:雷帕霉素靶蛋白TOR(Target of Rapamycin),是一种从酵母到哺乳动物高度保守的蛋白激酶。TOR是细胞感应外界营养水平进而调节生长和衰老的中心调控子。TOR被发现可以调控核糖体发生、翻译起始、代谢、应激反应、自噬等等信号通路。从酵母中的TOR到哺乳动物中的mTOR,之前的研究大都集中于氨基酸和葡萄糖对TOR活性的调控作用。5月31日,来自哈佛医学院 Julia R. K

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PNAS#
98
#靶蛋白#
68
#抗真菌#
62
学习了谢谢分享
86
#真菌#
73
#真菌感染#
72
#新策略#
67
很好,值得关注
86
非常好的文章,学习了,很受益
95