J Asthma Allergy:手术在治疗鼻塞和控制哮喘中的作用
2020-12-26 AlexYang MedSci原创
大多数哮喘患者,无论是过敏性或非过敏性的,通常都会表现出某种水平的并发鼻炎。鼻炎和哮喘的治疗均会对两种疾病产生影响。
大多数哮喘患者,无论是过敏性或非过敏性的,通常都会表现出某种水平的并发鼻炎。鼻炎和哮喘的治疗均会对两种疾病产生影响。
最近,有研究人员调查了慢性鼻炎(CR)和哮喘患者在鼻腔阻塞手术后的哮喘特异性结果,并确定最有可能在手术后能够改善哮喘控制的患者群体。研究人员前瞻性地招募了患有CR和鼻阻塞的哮喘患者,评估了鼻阻塞手术前和手术后的鼻腔和哮喘特定结果。研究共包括了28名参与者。在术前和术后3个月的评估中发现,哮喘控制测试(ACT)和鼻腔鼻窦结果测试-22评分之间存在显著关联。鼻腔手术后表现出ACT改善的患者术前ACT评分和预测的1秒内强迫呼气量更差。
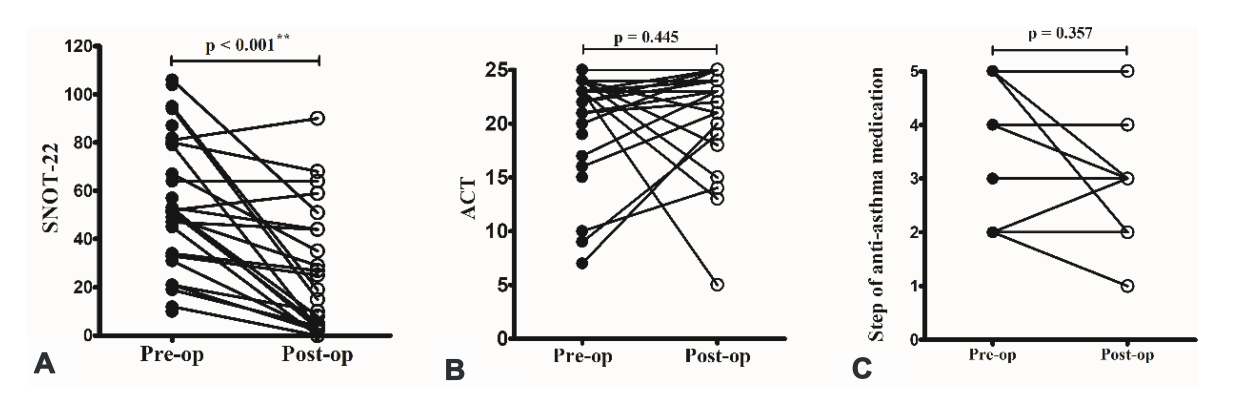
鼻手术改善鼻腔鼻窦症状(A),而不改善哮喘控制(B),以及哮喘控制药物使用情况(C)
最后,研究人员指出,鼻部症状严重程度与CR和鼻腔阻塞的哮喘患者的哮喘控制程度密切相关。对控制不佳的哮喘患者进行CR和鼻阻塞的评估应考虑作为为改善治疗响应和患者生活质量的重要方法。
原始出处:
Pei-Wen Wu , Ta-Jen Lee , Chun-Hua Wang et al. The Role of Surgery in Treating Nasal Obstruction to Control Asthma. J Asthma Allergy. 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AST#
57
#asthma#
54
#ALL#
52
#鼻塞#
70
很好的文章,学习了
115
学习了。
146
好文章!
101