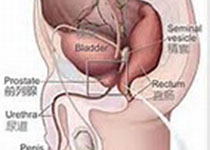
Prostate Cancer P D:PCA3和TMPRSS2:ERG 泌尿生物标记在预测活检结果中的表现分析
2019-02-01 AlexYang MedSci原创
对于那些前列腺癌积极监控的男性来讲,生物标记可能改善再分类预测到更高的等级或者体积癌症。最近,有研究人员调查了泌尿标记PCA3和TMPRSS2:ERG(T2:ERG)与基于活检的再分类之间的相关性。研究人员在基线时间点、6、12和24个月时收集了患者的尿液,并定量了PCA3和T2:ERG的水平。在分类定义为格林森得分的增加或者癌症活检核心比例不小于34%。调整了常见的临床变量后,研究人员还评估了生
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PRS#
63
#Prostate Ca#
65
#活检#
47
#生物标记#
49
#ROS#
59
#PRO#
55