Neurology:不同社区人群中轻度认知障碍事件的预测因素及其进程
2021-12-09 Naomi MedSci原创
近日,研究人员探讨轻度认知损害(MCI)事件发生的社会人口学和医学预测因素,包括持续MCI诊断、认知正常分类和进展为痴呆。近一半MCI诊断患者在随访时被归类为认知正常,其预测因子明显不同随后的病程。
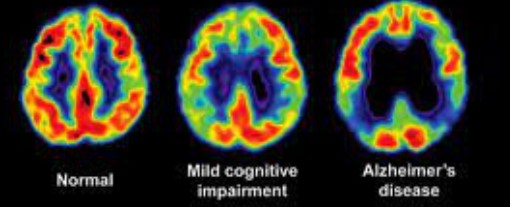
在认知正常的老年人中识别轻度认知障碍(MCI)的风险因素可以帮助确定痴呆预防或干预策略的目标群体。然而,并不是每个被诊断为MCI的人随后都会进展为痴呆症;纵向研究表明,在一次就诊时被确认为MCI的人中,有5-53%的人在下一次就诊时不再符合MCI标准。因此,在被诊断为MCI事件的个人中,确定进展为痴呆症的风险因素是平等的。
MCI的诊断通常基于Petersen标准,使用认知损害和日常功能的分界值。MCI的诊断还可以通过受影响的认知域的类型(即健忘型与非健忘型)和数量(即单域与多域)来进一步表征。虽然MCI标准要求相对保持日常功能,但先前的研究表明,MCI患者在日常功能活动方面比认知正常的人更困难,特别是在多域MCI的情况下。
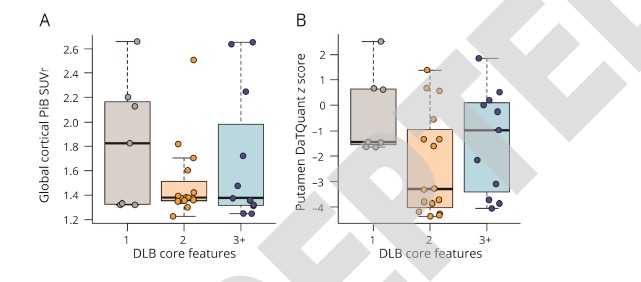
既往研究报告了在多种族社区队列中流行的MCI进展的预测因素。近日,有研究人员调查非西班牙裔白人、非西班牙裔黑人和西班牙裔认知正常者中发生MCI的可改变和不可改变的危险因素,探讨轻度认知损害(MCI)事件发生的社会人口学和医学预测因素,包括持续的MCI诊断、认知正常分类和进展为痴呆。
在以社区为基础的队列中,使用已发表的算法进行MCI的诊断。痴呆症的诊断是基于临床共识。Cox回归估计与几个预测因素相关的事件MCI的危险比。修正的Poisson回归估计了与发病后随访的诊断状态预测因素相关的相对风险。
- 在2903名基线认知正常的参与者中,752人在平均6.3年(SD=4.5)的时间内患上了MCI(发病率:56/1000人年)。
- APOEε4的存在和较高的医疗负担增加了发生轻度认知障碍的风险,而更多的教育年限,更多的休闲活动和更高的收入降低了这种风险。
- 在发生的MCI病例中,平均随访2.4年,12.9%进展为痴呆,9.6%功能下降,不符合MCI算法标准,但也不符合痴呆临床标准,29.6%继续符合MCI标准,47.9%不再符合MCI标准。
- 多域认知障碍、载脂蛋白Eε4的存在、抑郁症状和抗抑郁药物的使用增加了进展为痴呆症的风险。
这项以社区为基础的研究表明,几乎一半的MCI事件诊断患者在随访时被归类为认知正常。事件MCI的预测因子明显不同于随后的MCI病程;这些发现可以提炼MCI患者对认知和功能过程的预期。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Neurol#
72
学习了
106
学习学习
87
#预测因素#
67
#社区#
80