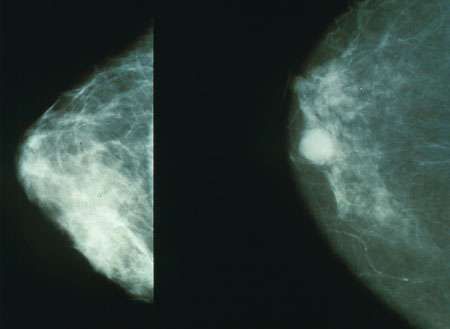
JNCI:新型疗法或有望治疗恶性三阴性乳腺癌亚型
2017-01-08 佚名 生物谷
图片摘自:3d-pictures.picphotos.net 最近,一项刊登在国际杂志the Journal of the National Cancer Institute上的研究报告中,来自休斯顿卫理公会医院(Houston Methodist Hospital)的研究人员通过研究开发出了一种治疗组织转化型乳腺癌的潜在疗法,这种乳腺癌是一种三阴性乳腺癌的恶性亚型疾病,患者的生存期不到4

图片摘自:3d-pictures.picphotos.net
最近,一项刊登在国际杂志the Journal of the National Cancer Institute上的研究报告中,来自休斯顿卫理公会医院(Houston Methodist Hospital)的研究人员通过研究开发出了一种治疗组织转化型乳腺癌的潜在疗法,这种乳腺癌是一种三阴性乳腺癌的恶性亚型疾病,患者的生存期不到4年。
文章中,研究者鉴别出了一种驱动组织转化型乳腺癌发生的关键基因,研究者Chang说道,我们不仅揭开了刺激癌症生长的生化通路,还发现了能够阻断该通路的化合物,这就能够有效增加携带人类组织转化型乳腺肿瘤的小鼠的生存期。
组织转化型乳腺癌在所有乳腺癌类型中占比不到1%,其实三阴性乳腺癌的一种恶性亚型疾病,如今并没有有效的疗法来对组织转化型乳腺癌进行治疗,由于这类癌症对化疗具有较高的无应答性,因此患者三年的生存率往往低于40%,甚至比三阴性乳腺癌患者70%的生存率还要低,因此鉴别出关键的遗传突变对于研究者开发新型疗法抵御这类癌症就显得尤为重要。
文章中,研究者在组织转化型乳腺癌患者的40份肿瘤样本中发现39份样本都携带有相同的基因突变,突变的基因名为RPL39,该基因类似于HER2基因(HER2基因在五分之一的乳腺癌患者机体中都处于过表达状态),被认为是一种癌基因,这就意味着,携带错误基因RPL39的细胞就会分裂失控快速诱发肿瘤产生,而鉴别出RPL39基因也仅仅是研究者攻克组织转化型乳腺癌的第一步。
RPL39基因能够调节诱导型一氧化氮合酶(inducible nitric oxide synthase, iNOS)的表达,研究人员发现,携带较高水平RPL39和iNOS的患者的总体生存率往往较低,为此研究人员调查了iNOS抑制剂对于治疗组织转化型乳腺癌的效果,结果发现,L-NMMA化合物能够促进携带小鼠机体的肿瘤发生萎缩。
最后研究者Chang说道,本文研究结果表明,结合标准化化疗或许有望治疗携带人类乳腺肿瘤的小鼠;我们的研究目标就是将组织转化型乳腺癌从一种顽疾变成临床上可控的慢性疾病,目前研究人员正在招募志愿者进行L-NMMA化合物治疗组织转化型乳腺癌的1期临床试验。
原始出处
Bhuvanesh Dave, Daniel D. Gonzalez, Zhi-Bin Liu, Xiaoxian Li, Helen Wong, Sergio Granados, Nadeer E. Ezzedine, Douglas H. Sieglaff, Joe E. Ensor, Kathy D. Miller, Milan Radovich, Agda KarinaEtrovic, Steven S. Gross, Olivier Elemento, Gordon B. Mills, Michael Z. Gilcrease and Jenny C. Chang.Role of RPL39 in Metaplastic Breast Cancer.JNCI.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新型疗法#
75
#阴性乳腺癌#
71
#NCI#
66
#三阴性#
67
携带较高水平RPL39和iNOS的患者的总体生存率往往较低
108
这类癌症对化疗具有较高的无应答性,因此患者三年的生存率往往低于40%,甚至比三阴性乳腺癌患者70%的生存率还要低
104
组织转化型乳腺癌
112