新解剖发现!第五肋间前血管对保留乳头的乳房切除术的重要性
2022-03-09 MedSci原创 MedSci原创
研究者描述了第五肋间前动脉穿支的血管解剖及其在保留乳头乳房切除术后灌注乳头乳晕复合体中的作用。
优化乳腺切除术已经成为乳腺外科医生的新标准。优化定义为最大程度的实质切除,保留未受影响的皮下组织,并尽量减少乳腺切除术皮瓣的破坏。
另一个优化指标则是保留乳头的乳房切除术,这有助于提高目前通常取得的效果。
优化乳腺切除的首要任务是了解乳房、乳头-乳晕复合体和周围结构的血管解剖,以最大限度地降低缺血性并发症和坏死的风险。

图1 文章来源
研究者描述了第五肋间前动脉穿支的血管解剖及其在保留乳头乳房切除术后灌注乳头乳晕复合体中的作用。
该研究主要采用20具新鲜尸体经内乳动脉注入20cc彩色乳胶。
移除肋骨后,将导管放置在第二肋间的水平位置。研究者在放大镜下解剖第五肋间间隙,观察第五肋间前动脉穿支的起源和运动轨迹,并对第五肋间动脉穿支进行了六次选择性CT血管造影。
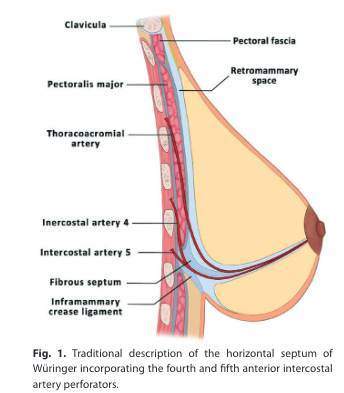
图2Würinger水平中隔的传统描述包括第四和第五肋间前动脉穿支
除此外,该文还报道了一例乳腺肥大患者行保留乳头乳房切除术的临床病例,以证明保留第五肋间前动脉穿支的有效性。
结果显示,所有病例均观察到第五肋间前动脉穿支,并经血管造影证实,具体显示产生了几个向各个方向移动的分支。
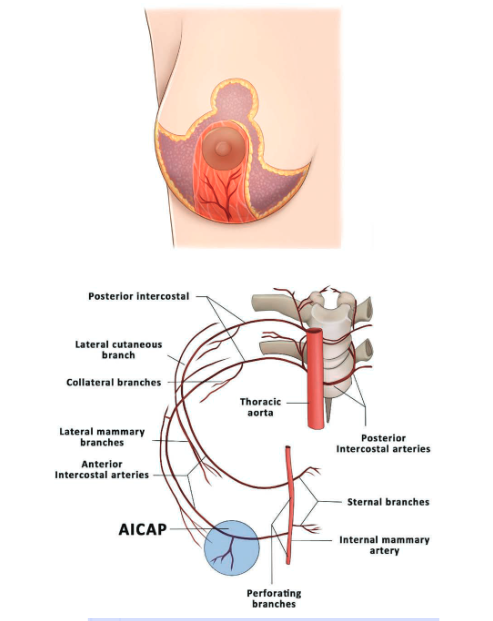
图3上图)下蒂示意图,包括第五肋间前动脉穿支。(下图)选择性血管造影显示的第五肋间前动脉穿支(AICAP)向乳头乳晕复合体(针)延伸。
第五肋间前动脉穿支的升支指向乳头复合体,走行于皮肤和实质之间的皮下层。第四和第五肋间前动脉穿支相互独立。

图4根据尸体研究观察解剖学,其中第四和第五肋间前动脉穿支通过不同路径向乳头-乳晕复合体上升
皮肤和乳头乳晕复合体保留乳房切除术的解剖学基础已通过CT血管造影、尸体和临床实例进行了描述。第五肋间前动脉穿支的主要升支通过皮下组织独立于Würinger水平中隔到达乳头乳晕复合体。对于这个重要的解剖发现,研究者建议外科医生认识到第五肋间前动脉穿支对乳头-乳晕复合体的灌注有重要作用。
原始文章:
Nahabedian, Maurice, Angrigiani, Claudio, Rancati, Alberto, Irigo, Marcelo, Acquaviva, Juan, Rancati, Agustin. The Importance of Fifth Anterior Intercostal Vessels following Nipple-Sparing Mastectomy. Plast Reconstr Surg. 2022;149(3):559-566. doi:10.1097/PRS.0000000000008828.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#切除术#
113
学习
105
#重要性#
114
学习
0
学习
114