BioMarin公司血友病基因疗法Ⅲ期临床5年的长期效果观察,数据积极
2022-01-16 网络 网络
BioMarin的疗法,称为valoctocogene roxaparvovec或'valrox',在第3阶段GENER8-1试验中,20名严重A型血友病成人患者中,8名凝血因子VIII的水平得到充分
BioMarin的疗法,称为valoctocogene roxaparvovec或'valrox',在第3阶段GENER8-1试验中,20名严重A型血友病成人患者中,8名凝血因子VIII的水平得到充分改善,满足了预先规定的监管审查标准。
2019年6月,BioMarin报告了其针对A型血友病基因疗法的三年数据,该数据用于支持其在欧洲和美国的申请,然而,其长期治疗价值也引起了质疑。详细见:BioMarin的血友病基因疗法III期临床达到终点,但其长期效应引起质疑
2022年1月9日,BioMarin Pharmaceutical公司宣布,valoctocogene roxaparvovec在一项正在进行的Ⅲ期临床试验中获得积极结果。
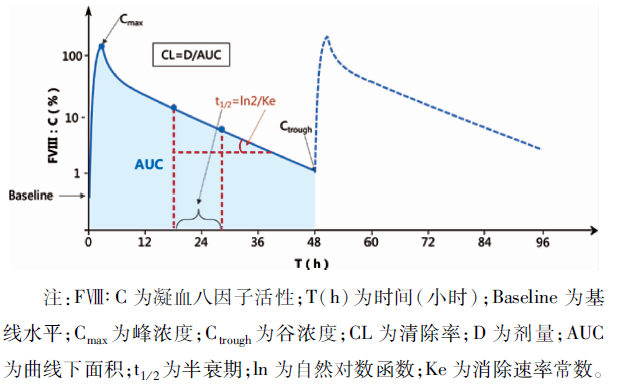
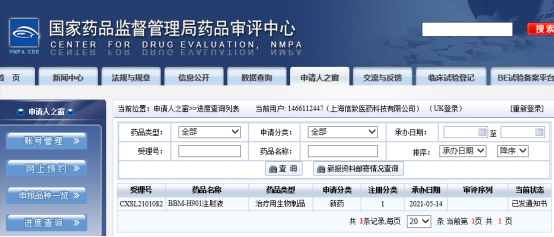
这是一款使用AAV5病毒载体,递送表达凝血因子VIII的转基因的在研基因疗法,用于治疗严重血友病A成人患者。试验结果表明,在112名受试者(中位随访时间为110周)中,与4.8的基线值相比,valoctocogene roxaparvovec使患者年出血率(ABR)降低85%。在整个评估期间,平均ABR为0.8。同时,该疗法使每年凝血因子VIII输注率较基线数据显著降低98%。在凝血因子VIII活性水平方面,第二年结束时,改良意向治疗(mITT)人群(n=132)的受试者中使用发色底物(CS)检测获得的平均内源性凝血因子VIII活性水平为23(中位数11.8)IU/dL,一步法(OS)检测获得的平均内源性凝血因子VIII活性水平为36.1(中位数21.6)IU/dL。n该疗法已经获得美国FDA授予的再生医学先进疗法认定(RMAT)和突破性疗法认定。基于试验数据,BioMarin计划在2022年第二季度重新向FDA递交生物制品许可申请(BLA)。
不过,也看到随着随访时间延长,FVIII的活性在持续降低。

不过,这项基因治疗一旦问世,将具有高昂的价格,详细见:BioMarin计划为其A型血友病基因疗法Valrox,定价为200万至300万美元
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Bio#
83
我记得之前看过一个用脂质体做载体的,想不太起来了
106
#长期效果#
91
#Ⅲ期临床#
86
#BioMarin#
94