ACC 2016:α硫辛酸不能降低PCI中对比剂的肾损伤发生率(CARIN)
2016-04-05 Mechront 译 MedSci原创
美国心脏病学年会上称,一种新型改良的α硫辛酸不能有效的防止PCI中对比剂诱导的肾脏损伤。布莱根妇女医院心血管介入项目的执行董事Bhatt博士说:“糖尿病或肾病患者进行PCI时,对比剂诱导的肾损伤是常见的问题,现有的有效疗法是预水化。当前有很多尝试降低造影剂对肾脏损害的工作,但是目前造影前水化仍是最佳方案,当前我们迫切的需要新的治疗方法。”CARIN试验中,Bhatt和同事评估看一种新型α-硫辛酸的
美国心脏病学年会上称,一种新型改良的α硫辛酸不能有效的防止PCI中对比剂肾病。
布莱根妇女医院心血管介入项目的执行董事Bhatt博士说:“糖尿病或肾病患者进行PCI时,对比剂诱导的肾损伤是常见的问题,现有的有效疗法是预水化。当前有很多尝试降低造影剂对肾脏损害的工作,但是目前造影前水化仍是最佳方案,当前我们迫切的需要新的治疗方法。”
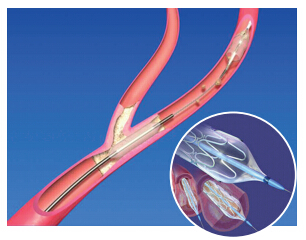
CARIN试验中,Bhatt和同事评估看一种新型α-硫辛酸的衍生物CMX-2043(Ischemix LLC)的安全性和有效性,该药物已被证明在支架过程中具有心脏保护作用。
该研究纳入了361名安排血管造影、有肾功能损伤且至少一个危险因素的患者,随机分为CMX-2043 (2.4 mg/kg、3.6 mg/kg或2.4 mg/kg给药2次,间隔24小时)和安慰剂组。
该研究以急性肾脏损伤的降低作为主要结局。次要终点包括MACE、主要肾脏不良事件、心脏损伤减少和4A型MI发生率降低。研究人员还记录了与治疗相关的不良事件。
数据显示,与安慰剂组相比,3个不同剂量CMX-2043组主要肾脏损伤事件的发生率较高,但无统计学意义(安慰剂组、2.4 mg/kg单剂量组、3.6 mg/kg 单剂量、2.4 mg/kg 双剂量组的发生率分别为:38.2%、 48.2%、55.6%、 46.3%。3.6 mg/kg vs. 安慰剂,P < .01;其余 > .1)。
研究者说:“所有小组的肾脏事件发生率都非常高,20%~30%的患者在3个月时因肾脏问题再次住院,药物的使用并不能降低高发生率。”
Bhatt说:“不同组之间的终点指标均无统计学显著差异。”
研究者总结说:“PCI所致急性肾损伤仍是一个大问题,高危患者的发生率约为20%~25%。不过本研究进行的药物试验并没有降低肾损伤的发生。现在我们无法确认之前提出的α硫辛酸的心脏保护作用。未来还需要对PCI所致急性肾损伤进行更大更透彻的研究。”
原始出处:
Bhatt DL, et al. Joint ACC/New England Journal of Medicine Late-Breaking Clinical Trials. Presented at: American College of Cardiology Scientific Session; April 2-4, 2016; Chicago.
CARIN: Novel drug does not prevent kidney injury from contrast during PCI.Healio.April 4, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发生率#
53
#ACC#
45
#损伤#
61
学习了,很好
155
在一个问题上深挖,挖,挖。
150