JAHA:外周动脉粥样硬化亚临床指标与新发房颤风险的关系
2022-01-03 MedSci原创 MedSci原创
外周动脉粥样硬化(颈动脉粥样硬化和下肢外周动脉粥样硬化)的基线和纵向亚临床指标与新发AF的风险增加显著相关,尤其是在女性中。
心房颤动(AF)是最常见的心律失常。随着人口老龄化,预计未来几年AF的患病率将急剧增加。尽管AF患者的治疗有所改善,但它仍然具有很高的发病率和死亡风险。但关于外周动脉粥样硬化的亚临床指标与新发AF之间(性别特异性)联系的基于人群数据十分有限。
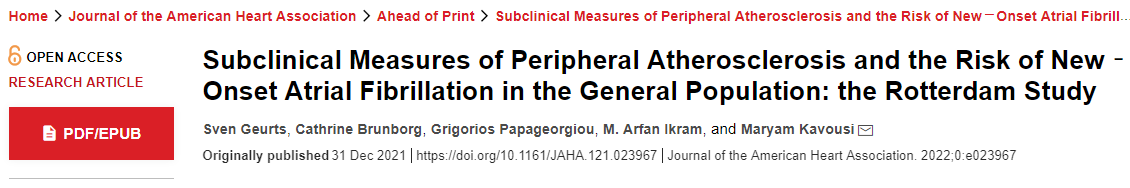
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在基线和随访中评估了外周动脉粥样硬化的亚临床指标,包括颈动脉内中膜厚度(cIMT)、颈动脉斑块和踝臂指数(ABI)。
该研究共有12840名来自鹿特丹研究且在基线时没有AF的参与者被纳入。根据心血管危险因素进行调整后,Cox比例风险模型和联合模型用于确定cIMT、颈动脉斑块和ABI的基线和纵向测量值与新发AF之间的关联。
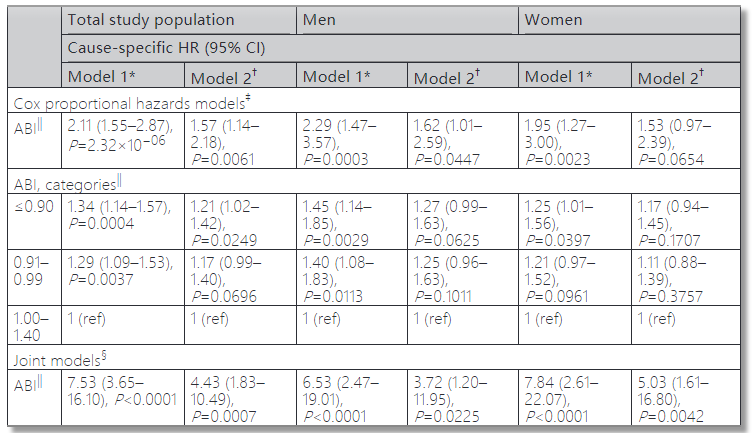
在9.2年的中位随访期间,12840名参与者(平均年龄为65.2岁,58.3%为女性)发生了1360例AF事件。基线较高cIMT(完全调整的风险比[HR],95%CI为1.81、1.21-2.71;P=0.0042),存在颈动脉斑块(完全调整的HR,95%CI为1.19、1.04-1.35;P=0.0089)、较低的ABI(完全调整后的HR,95%CI为1.57、1.14-2.18;P=0.0061)和较高cIMT的纵向测量值(完全调整后的HR,95%CI为2.14、1.38-3.29;P=0.02))、伴有颈动脉斑块(完全调整后的HR,95%CI为1.61、1.12-2.43;P=0.0112)和较低的ABI(完全调整后的HR,95%CI为4.43、1.83-10.49;P=0.0007)与一般人群新发AF显著相关。性别分层分析表明,cIMT、颈动脉斑块和ABI的关联在女性中最为突出。
由此可见,外周动脉粥样硬化(颈动脉粥样硬化和下肢外周动脉粥样硬化)的基线和纵向亚临床指标与新发AF的风险增加显著相关,尤其是在女性中。
原始出处:
Sven Geurts,et al.Subclinical Measures of Peripheral Atherosclerosis and the Risk of New‐Onset Atrial Fibrillation in the General Population: the Rotterdam Study.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.023967
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#粥样硬化#
117
#风险的关系#
63
学习了
81
粥样硬化在心脏中作用是相互的
86
#AHA#
58
#新发房颤#
103
#房颤风险#
56
#外周动脉#
74
学习学习
78
学习
110