J Leuk Biol:帮助HIV进入大脑的“特洛伊木马”
2015-02-05 佚名 生物谷
尽管大家都知道HIV在感染初期可以进入患者的大脑中,引发炎症和记忆认知问题,但是具体是如何发生的却无人知晓。近日,一篇发表于国际杂志Journal of Leukocyte Biology上的研究论文中,来自阿尔伯特-爱因斯坦医学院的研究人员通过研究揭示,HIV可以依赖于一种名为成熟单核细胞的免疫细胞表达的蛋白质来进入大脑,那么这种蛋白质或许是抑制HIV进入大脑细胞的一种新型药物靶点,尽管当前相关
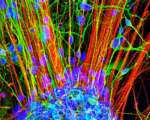
尽管大家都知道HIV在感染初期可以进入患者的大脑中,引发炎症和记忆认知问题,但是具体是如何发生的却无人知晓。近日,一篇发表于国际杂志Journal of Leukocyte Biology上的研究论文中,来自阿尔伯特-爱因斯坦医学院的研究人员通过研究揭示,HIV可以依赖于一种名为成熟单核细胞的免疫细胞表达的蛋白质来进入大脑,那么这种蛋白质或许是抑制HIV进入大脑细胞的一种新型药物靶点,尽管当前相关的研究较少,但研究者认为这位后期开发新型药物进入血脑屏障来治疗HIV感染提供了新的思路。
研究者Dionna W. Williams表示,我希望本文研究可以帮助开发靶向作用单核细胞流入大脑的辅助疗法从而来降低HIV进入到大脑中的水平,降低HIV相关的神经系统障碍的发生。
文章中,研究者从HIV感染和未感染的两类人群中收集血液进行分析,研究人员从两组研究对象的血液中分离出成熟的单核细胞,并且确定当前这些细胞的数量,表达蛋白的情况,同时对其进入大脑的特征进行研究分析;结果发现,成熟的单核细胞进入大脑中的能力取决于其特殊蛋白表达的量,这种特殊蛋白可以促进HIV对大脑的感染。
最后杂志主编John Wherry博士表示,单核细胞是人类机体抵御病毒感染的免疫系统的一份子,但是这些细胞或许也可以扮演“特洛伊木马”的角色来从原始感染位点将病毒携带到机体其它部位;本文研究鉴别出了成熟单核细胞协助HIV进入大脑的分子机理对于后期开发新型疗法来阻断HIV感染大脑及改善患者的生存率提供了新的研究依据和思路。
原始出处
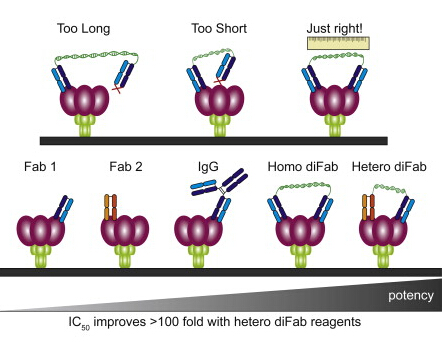
Williams DW1, Anastos K1, Morgello S1, Berman JW2.JAM-A and ALCAM are therapeutic targets to inhibit diapedesis across the BBB of CD14+CD16+ monocytes in HIV-infected individuals.J Leukoc Biol. 2015 Feb

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#特洛伊木马#
105
#Biol#
61
#Bio#
82
赞
156
已阅
176