武田在ASCO和EHA上展示肿瘤学产品组合和研发产品线的最新研究成果
2022-06-01 网络 网络
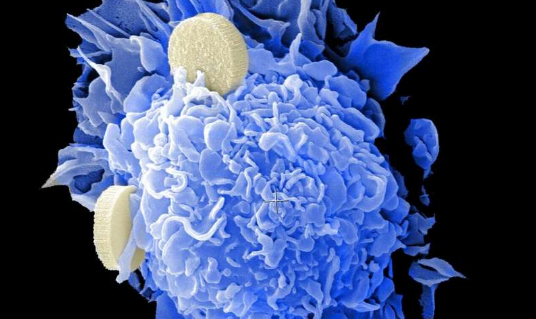
研发产品线报告重点阐述利用先天免疫力战胜癌症及改善患者生活的项目所取得的进展
武田药品工业株式会社(Takeda Pharmaceutical Company Limited, TSE:4502/NYSE:TAK)(简称“武田”)今天宣布,公司即将在今春举行的两次科学大会上公布数据,分别是6月3日至7日在伊利诺斯州芝加哥举行的第58届美国临床肿瘤学会年会(ASCO)和6月9日至12日在奥地利维也纳举行的第30届欧洲血液学协会会议(EHA)。武田在肿瘤学方面的最新研究侧重于加强和改善病人护理,同时为治疗方法有限的病人探索新方法。
武田公布的数据涉及一系列癌症,包括淋巴瘤、白血病、多发性骨髓瘤和非小细胞肺癌,以及针对利用先天免疫系统的研究性疗法的早期见解。
武田肿瘤细胞疗法和治疗领域部门负责人Christopher Arendt博士表示:“我们即将在今年春季的医学大会上公布的数据彰显出我们追求战胜癌症的目标,以及我们有能力与合作伙伴合作,以进一步提高研究能力。除了分享与目前已批准疗法相关的数据外,我们还将介绍公司先天免疫临床项目中的早期发现——其中许多项目正在探索新的作用机制。我们相信这些项目有能力推动肿瘤学领域的发展,并提升当前的护理标准。”
武田对肿瘤学的承诺
我们的核心研发使命是通过我们对科学、突破性创新和改善患者生活的激情的承诺,向全世界癌症患者交付新型药品。无论是凭借我们的血液治疗药物、我们强大的产品线,还是实体瘤药物,我们的宗旨是保持创新和竞争力,以便向患者提供他们需要的治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#最新#
63
#ASC#
64
#研究成果#
80
#研发#
74
#肿瘤学#
61
#武田#
68
#EHA#
75