Int J Surg Case Rep:肾细胞癌来源的甲状腺癌一例
2014-12-04 MedSci MedSci原创
Int J Surg Case Rep:肾细胞癌来源的甲状腺癌一例 这是来自伊朗的一篇病例报告:一58岁男性因发现快速生长的左侧颈部肿物伴随疼痛3月就诊,追问病史得知1.5年前曾因低分化肾细胞癌(RCC)行左肾切除术,临床分期为T1bN2M0,体检触及甲状腺左叶8*6cm肿块,查甲状腺功能在正常范围,颈部超声提示甲状腺左叶9*7cm低回声结节,无微钙化及囊性成分,腹部超声提示肝左右叶多发低回
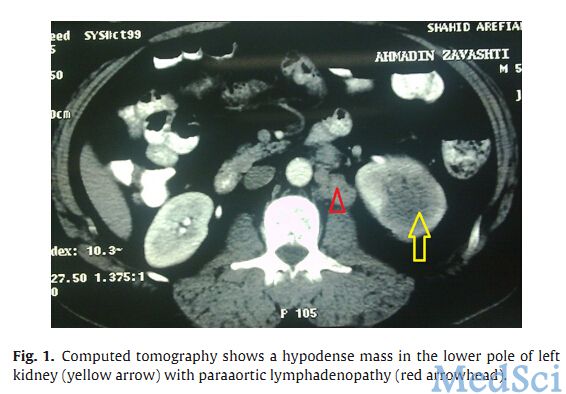

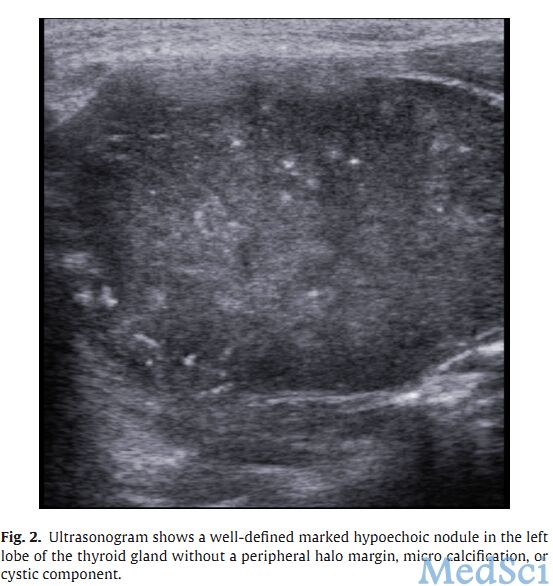
这是来自伊朗的一篇病例报告:一58岁男性因发现快速生长的左侧颈部肿物伴随疼痛3月就诊,追问病史得知1.5年前曾因低分化肾细胞癌(RCC)行左肾切除术,临床分期为T1bN2M0,体检触及甲状腺左叶8*6cm肿块,查甲状腺功能在正常范围,颈部超声提示甲状腺左叶9*7cm低回声结节,无微钙化及囊性成分,腹部超声提示肝左右叶多发低回声圆形结节(1-3cm),细针穿刺细胞学提示单层恶性腺细胞,伴颗粒细胞质,呈多形核,核内有假包涵体,复合肾细胞癌转移。
肾细胞癌来源的甲状腺转移在临床上实属罕见,原因在于甲状腺含高碘、高氧含量、高速血流,因此可有效防止肿瘤细胞定植,但是上述环境遭到破坏(比如甲状腺肿或甲状腺炎)。甲状腺就会受到转移肿瘤的侵袭。
以往的研究提示肾细胞癌在术后20年都有可能转移至甲状腺,细针穿刺细胞学检查对于检查甲状腺转移癌有很高的灵敏度和特异度,外科切除甲状腺转移癌并不能提高中位生存率,因此临床医生要详细询问病史,遇到此类情况要考虑是否有恶性肿瘤病史,准确诊断。
原文出处:
Mohammadi, A., S.B. Toomatari, and M. Ghasemi-Rad, Metastasis from renal cell carcinoma to thyroid presenting as rapidly growing neck mass. Int J Surg Case Rep, 2014. 5(12): p. 1110-1112.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








着。。。神奇
208
#case#
74
#细胞癌#
72
#Cas#
65