Stroke:24小时血管通畅与临床结局和梗死体积的相关性
2017-03-19 MedSci MedSci原创
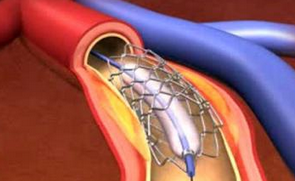
近期一些随机试验中观察到,与对照组相比,24小时靶血管通畅率在血栓切除术组中更高。近期,一项发表在杂志Stroke上的研究旨在评估治疗组和闭塞位置的24小时血运重建率,因为它们与REVASCAT(前循环的大血管阻塞在症状发作的8小时内呈现的急性中风,比较FR装置与最佳医疗治疗的血管再生的随机对照试验)的临床结果和24小时梗死体积相关。此项研究根据计算机断层扫描/磁共振(94.2%/ 5.8%)血管
近期一些随机试验中观察到,与对照组相比,24小时靶血管通畅率在血栓切除术组中更高。
近期,一项发表在杂志Stroke上的研究旨在评估治疗组和闭塞位置的24小时血运重建率,因为它们与REVASCAT(前循环的大血管阻塞在症状发作的8小时内呈现的急性中风,比较FR装置与最佳医疗治疗的血管再生的随机对照试验)的临床结果和24小时梗死体积相关。
此项研究根据计算机断层扫描/磁共振(94.2%/ 5.8%)血管造影术显示的24小时改良动脉闭塞性病变及计算机断层扫描上24小时梗死体积进行分类,研究独立核心实验室判断的血管状态(血栓切除组中95/103例vs.对照组中94/103)。完全血运重建定义为改良的动脉闭塞病变3级。通过序数逻辑回归分析其对临床结果的影响。
在血栓切除术组(调整的优势比,4.5; 95%置信区间,1.9-10.9)和对照组中(调整的优势比,2.7; 95%置信区间,1.0-6.7),均出现完全血运重建与改善的结果相关。两组中,血运重建(改良的动脉闭塞性损伤2/3)均与较小的梗死体积相关。
此项研究结果表明:在24小时出现的完全血运重建是临床结果的有力预测证据;在血栓切除术和对照组中,任何类型的血运重建均可以减少的梗死体积。
原始出处:
Millán M, Remollo S, et al. Vessel Patency at 24 Hours and Its Relationship With Clinical Outcomes and Infarct Volume in REVASCAT Trial (Randomized Trial of Revascularization With Solitaire FR Device Versus Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting Within Eight Hours of Symptom Onset). Stroke. 2017 Mar 14. pii: STROKEAHA.116.015455. doi: 10.1161/STROKEAHA.116.015455.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#相关性#
84
#临床结局#
70
#24小时#
66
学习了……
126
签到学习了很多。
104