结果令人鼓舞,肿瘤电场治疗联合标准化疗作为胃癌一线治疗的2期临床研究EF-31达到主要终点
2022-06-11 “生物世界”公众号 “生物世界”公众号
再鼎医药与 Novocure 公司联合宣布,肿瘤电场治疗联合标准化疗作为胃癌一线治疗的2期临床研究EF-31达到主要研究终点客观缓解率,次要研究终点均显示积极信号。
近日,再鼎医药与 Novocure 公司联合宣布,肿瘤电场治疗联合标准化疗作为胃癌一线治疗的2期临床研究EF-31达到主要研究终点客观缓解率,次要研究终点均显示积极信号。
经肿瘤电场治疗联合标准化疗治疗的患者确认客观缓解率为50%
缓解持续时间为10.3个月
一年生存率为72%
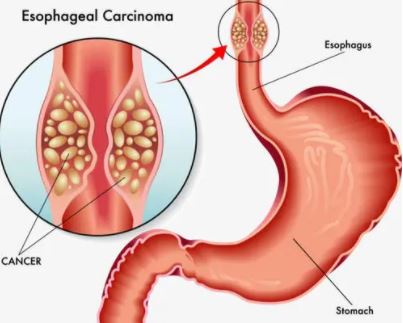
该临床研究旨在评估肿瘤电场治疗(TTFields)联合标准治疗(化疗单药或联合曲妥珠单抗用于治疗HER-2阳性患者)作为胃腺癌一线治疗的有效性及安全性。肿瘤电场治疗耐受性良好,在XELOX化疗或联合方案治疗中没有增加系统性毒性,没有高级别皮肤毒性上报。
初期分析在中位随访时间8.6个月后开展。主要研究终点确认的客观缓解率为50%,中位无进展生存期为7.8个月,缓解持续时间为10.3个月。中位总生存期未达到,一年生存率为72%。
同济大学附属东方医院肿瘤医学部主任李进教授表示:"针对这种历来难治的瘤种,EF-31的结果令人鼓舞。在标准化疗方案中联合肿瘤电场治疗,对胃癌患者的治疗产生积极影响,期待在后续的临床研究中证实这些数据。"
EF-31临床研究是一项在中国开展的前瞻性、单臂2期临床研究。该研究纳入了26例未接受过系统性治疗的无法切除、局部进展或转移性的胃食管交界部癌或胃腺癌患者。患者接受了肿瘤电场治疗联合XELOX化疗(奥沙利铂联合卡培他滨)的持续治疗。HER2阳性患者允许使用曲妥珠单抗。
再鼎医药总裁、肿瘤领域全球开发负责人 Alan Sandler 博士表示:"在全球,每年有超过100万人确诊胃癌,大约一半发生在中国,改善治疗方案迫在眉睫。在中国开展的EF-31研究是Novocure与再鼎医药共同拓展肿瘤电场治疗进入新疾病领域的重要里程碑。我们期待与Novocure在未来多个实体肿瘤适应症的全球临床研究中继续合作。"
Novocure 首席执行官 Asaf Danziger 表示:"肿瘤电场治疗是一项高度通用型的物理治疗方案,在实体肿瘤与治疗领域具有广泛适用的潜力。非常感谢我们的患者、研究者以及合作伙伴再鼎医药。EF-31研究表明了在标准治疗中加入肿瘤电场治疗将有望改善胃癌患者的预后。我们迫不及待地希望继续探索这些潜在获益,推进到随机的3期临床研究。"
肿瘤电场治疗(Tumor Treating Fields,TTFields)是一种利用特定电场频率干扰细胞分裂,抑制肿瘤增长并使受电场影响的癌细胞死亡的癌症治疗手段。它是利用低强度、中频(100-300kHz)交流电场来干扰细胞的有丝分裂,从而诱导快速分裂细胞(比如癌细胞)的死亡。

使用肿瘤电场治疗的脑肿瘤患者
相比于健康细胞,癌细胞会迅速且不受控制得进行有丝分裂,因此可以调整肿瘤电场治疗的频率特异性地影响癌细胞,同时使健康细胞几乎不受影响。

肿瘤电场治疗原理示意图
在目前所有的临床前研究中,肿瘤电场治疗均显示出一致的抗有丝分裂作用。肿瘤电场治疗主要和其他标准治疗方案联用。有越来越多的体外证据支持肿瘤电场治疗能够广泛地与癌症治疗方案联用,例如放疗、部分化疗和部分免疫治疗。
迄今为止,在临床研究和商业化阶段中,肿瘤电场治疗未显示出系统性毒性,最常见副作用为轻中度的皮肤反应。肿瘤电场治疗全球研发计划涵盖了临床前合作和所有阶段的广泛临床研究,其中包括4个多个瘤种类型的3期关键性临床研究。迄今,已有超过24000名癌症患者使用了肿瘤电场治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#2期临床#
87
#标准化疗#
65
#标准化#
59
#主要终点#
55
学习了
70
#肿瘤电场治疗#
53