Journal for ImmunoTherapy of Cancer:CTLA-4及OX40双特异性抗体ATOR-1015的临床前数据
2019-04-13 不详 网络
Alligator Bioscience公司近日宣布,CTLA-4及OX40双特异性抗体ATOR-1015的临床前数据已经发表在《Journal for ImmunoTherapy of Cancer》杂志上。
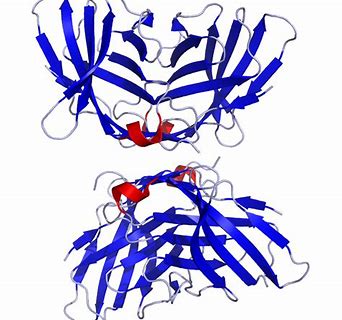
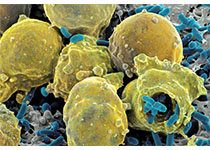
Alligator Bioscience公司近日宣布,CTLA-4及OX40双特异性抗体ATOR-1015的临床前数据已经发表在《Journal for ImmunoTherapy of Cancer》杂志上。已发表的数据显示,ATOR-1015在几种实验性肿瘤模型(包括膀胱癌,结肠癌和胰腺癌)中具有抗肿瘤作用。此外,数据表明ATOR-1015与PD-1阻断疗法的组合能够诱导长期免疫记忆以及增强的抗肿瘤反应。
该数据支持了ATOR-1015的持续临床开发,目前正在进行I期研究(NCT03782467),这项研究的结果预计将在2020年下半年公布。
原始出处:
http://www.firstwordpharma.com/node/1634983#axzz5kmtmGZrh
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床前数据#
60
#OX40#
77
#特异性#
47
#ERA#
66
#CTLA-4#
57
#特异性抗体#
47