Thromb Haemostasis:血小板周转可以预测冠状动脉介入治疗后患者预后?
2017-05-31 xing.T MedSci原创
总之,RPF作为血小板周转率的指标是PCI术后接受双抗治疗患者发生MACE和出血事件的独立预测因素。由于RPF可以可靠地量化以及连同常规血象,RPF可能很容易被应用于预测心血管风险。
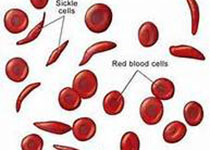
升高的血小板周转率导致血小板高反应性。经皮冠状动脉介入治疗(PCI)后血小板高反应性与主要心血管不良事件(MACE)相关。近日,血栓和凝血疾病权威杂志Thrombosis and Haemostasis上发表了一篇研究文章,研究人员旨在明确PCI支架置入术后血小板周转率和功能对MACE的预测价值。
在这项前瞻性观察性研究中,486例连续就诊的进行PCI术且服用阿司匹林和氯吡格雷的患者被纳入研究,并且测定了血小板的周转率(平均血小板体积(MPV)、网织血小板分数(RPF))和血小板功能(多电极法(MEA)、血管舒张剂刺激磷蛋白磷酸化(VASP-P)法)。
在六个月的随访,10.7 %的病人发生MACE。RPF(比值比[OR]为1.173(95%可信区间[CI] 为1.040-1.324),P=0.009)和MPV(OR值为1.459(95%CI为1.059-2.008),P=0.021)是MACE的单变量预测因子,而VASP-P(OR为1.016(95%CI为1-1.032),P=0.052)和MEA(OR为0.999(95%CI为0.980-1.017),P=0.895)未能预测MACE的发生。RPF仍然是与MACE独立相关的唯一血小板指标。
最好的预测MACE的模型纳入了肌钙蛋白I(OR为1.007(95 %CI为1.002-1.012),P=0.009)、RPF(OR为1.136(95%CI为1.001-1.288),P=0.048)、CRP(OR为1.008(95%CI为1.001-1.014),P=0.023)和心肌梗死病史(OR为2.039(95%CI为1.093-3.806),P=0.025)。RPF(OR为1.211(95%CI为1.042-1.406),P=0.012)也与院内出血存在独立相关性。
总之,RPF作为血小板周转率的指标是PCI术后接受双抗治疗患者发生MACE和出血事件的独立预测因素。由于RPF可以可靠地量化以及连同常规血象,RPF可能很容易被应用于预测心血管风险。
原始出处:
M. K. Freynhofer,et al. Platelet turnover predicts outcome after coronary intervention.Thrombosis and Haemostasis.2017. https://th.schattauer.de/en/contents/archive/issue/2480/issue/special/manuscript/27239/show.html
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#患者预后#
91
#HAE#
65
#冠状动脉介入治疗#
91
#STAS#
71
学习啦谢谢分享
75
学习了,谢谢作者分享!
121
666沉迷于学习
91
学习啦谢谢分享
71