Blood:ALL儿童患者停用天冬酰胺酶后的复发风险
2020-11-17 MedSci原创 MedSci原创
天冬酰胺酶在急性淋巴细胞白血病(ALL)治疗中的重要作用已被明确。根据当下大多数方案治疗,ALL患儿的总体存活率已超过了90%,但天冬酰胺酶相关毒性仍是目前面临的一个重要问题,除了会引起急性死亡外,还
天冬酰胺酶在急性淋巴细胞白血病(ALL)治疗中的重要作用已被明确。根据当下大多数方案治疗,ALL患儿的总体存活率已超过了90%,但天冬酰胺酶相关毒性仍是目前面临的一个重要问题,除了会引起急性死亡外,还可能引起停药后的复发风险增加。
该研究在1401名1-17岁的儿童中调查了天冬酰胺酶暴露后的复发风险,这些儿童在2008年7月-2016年2月期间被诊断为ALL,并根据NOPHO ALL2008方案进行治疗,包括延长天冬酰胺酶暴露(5-33周肌肉注射1000IU/m2)。随访直到复发、死亡、继发性恶性肿瘤或随访结束(中位数时间 5.71年,四分位数范围:4.02-7.64)。
在多因素Cox模型中,比较因临床毒性而停用天冬酰胺酶治疗(n=358)和不使用天冬酰胺酶治疗(n=1043)的患者,调整后的复发特异性危险比(aHR)为1.33(95% CI:0.86-2.06,P=0.20)。
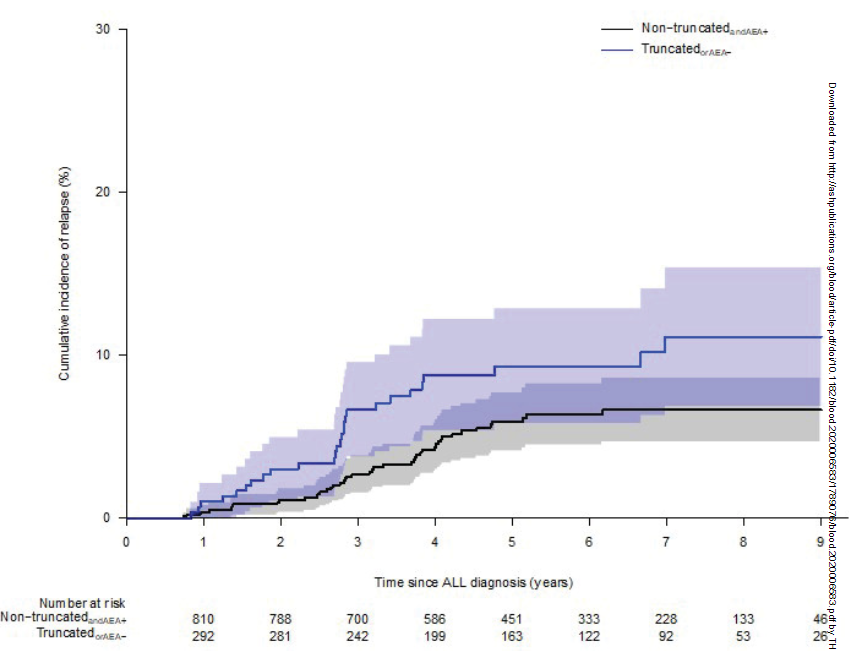
在一项只纳入有酶活性信息的患者的子研究中(n=1115),301名停用天冬酰胺酶治疗或天冬酰胺酶沉默失活(SI)的患者(157名超敏反应、53名胰腺炎、14名血栓形成、31名其他、46名SI)的7年累计复发率为11.1%(95% CI:6.9-15.4),而其余814名患者的为6.7%(4.7-8.6)。复发特异性aHR为1.69(95% CI: 1.05~2.74,P=0.03)。未调整的骨髓复发特异性HR分别为1.83 (95%CI:1.0 7~3.14,P=0.03)和1.86 (95%CI:0.90~3.87,P=0.095)。
综上所述,该结果强调了治疗药物监测的重要性,并在可行的情况下适当调整天冬酰胺酶治疗。
原始出处:
Gottschalk H?jfeldt Sofie,Grell Kathrine,Abrahamsson Jonas et al. Relapse risk following truncation of PEG-asparaginase in childhood acute lymphoblastic leukemia.[J] .Blood, 2020, undefined: undefined.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#复发风险#
55
#ALL#
72
收获
0
所以还缺少一些相关指南
102
了解
119
拜读了,写的不错
101