JAHA:内皮素预测小儿先天性心脏病相关肺动脉高压的严重程度
2021-10-09 刘少飞 MedSci原创
肺动脉高压(PAH)是一种严重的疾病,其特征是肺血管阻力(PVR)增加和肺血管重构,导致心力衰竭和死亡。 第六届世界肺动脉高压研讨会将第 1 组 PAH 定义为平均肺动脉压 (mPAP) >20

肺动脉高压(PAH)是一种严重的疾病,其特征是肺血管阻力(PVR)增加和肺血管重构,导致心力衰竭和死亡。 第六届世界肺动脉高压研讨会将第 1 组 PAH 定义为平均肺动脉压 (mPAP) >20 mm Hg、肺血管阻力指数 (PVRi) ≥3WU×m2 和肺毛细血管楔压 <15 mm Hg。由于有限的儿科特定数据和发育中的肺血管系统,了解儿科 PAH 具有挑战性。 小儿 PAH 与成人 PAH 不同,特发性 PAH、遗传性 PAH、遗传综合征和疾病相关 PAH,尤其是与先天性心脏病 (APAH-CHD) 相关的 PAH 的患病率更高。
研究目的:
血管生成抑制剂内皮抑素与成人更差的肺动脉高压 (PAH) 结果和儿童肺发育不良有关。本研究旨在评估内皮抑素是否与儿科 PAH 的疾病严重程度和结局相关。
研究方法和结果
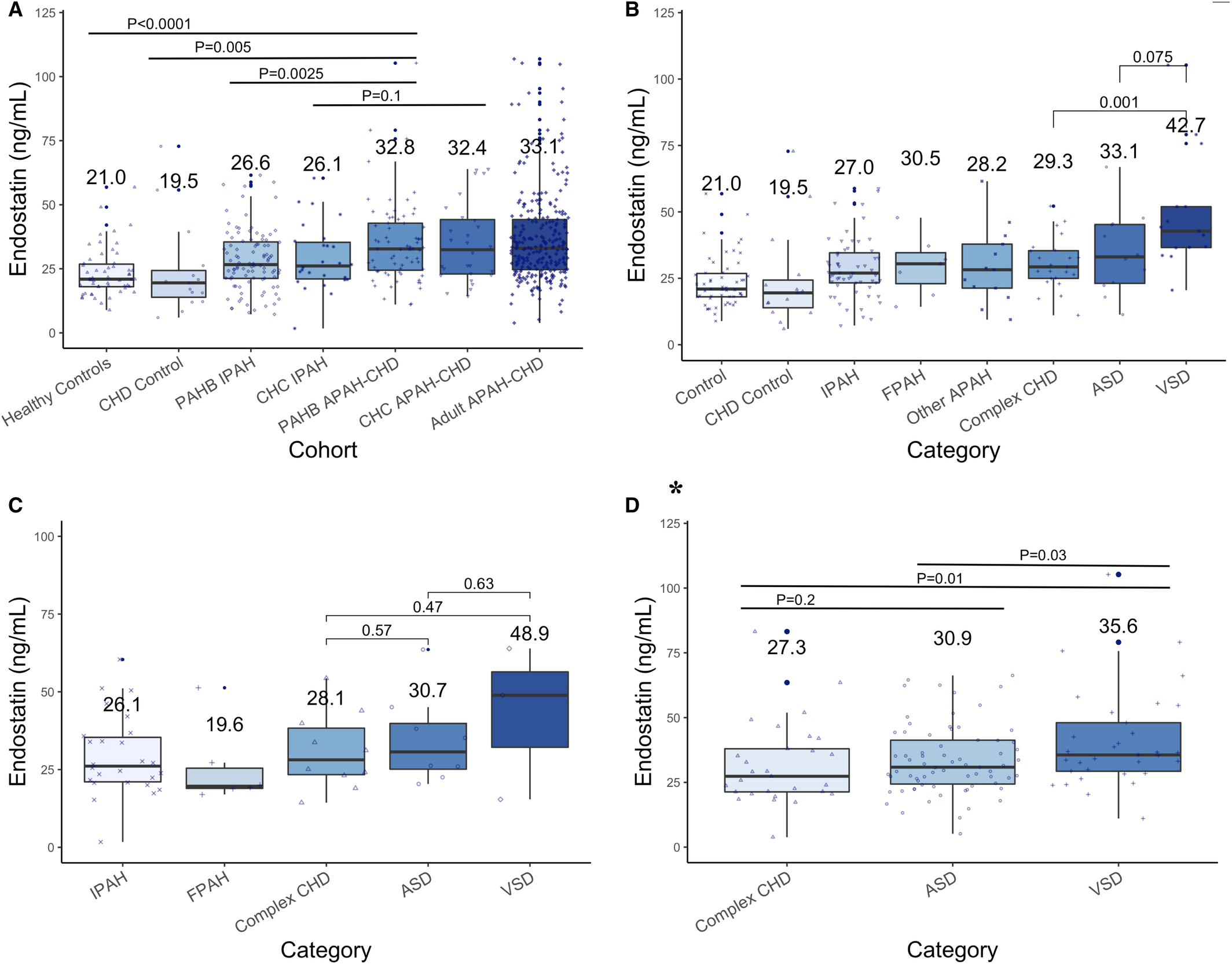
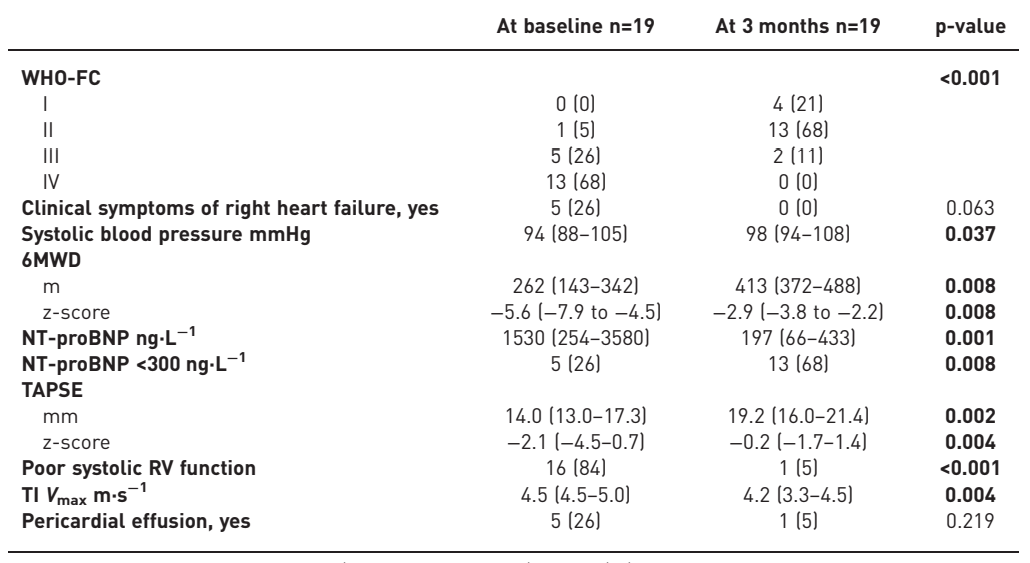
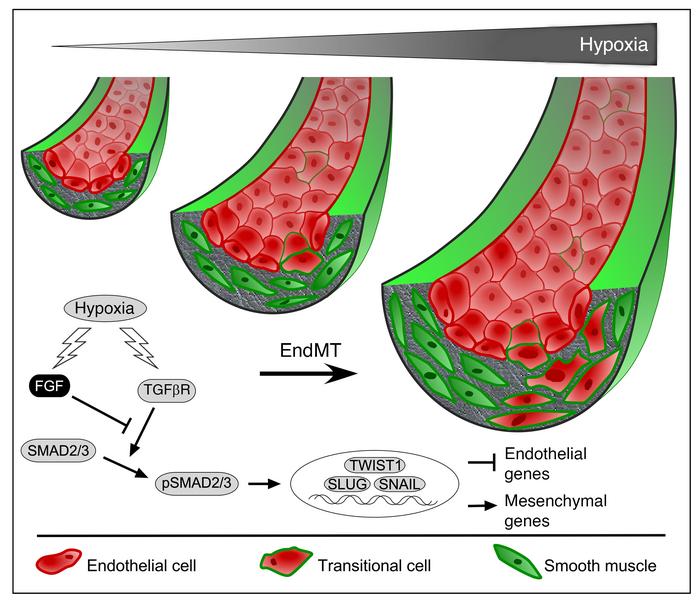
在患有 PAH 的儿科受试者、健康儿科对照和患有先天性心脏病 (CHD) 的儿科对照 (N=54, N=15) 的横断面 (N=160) 和纵向队列 (N=64) 中测量血清内皮抑素,和患有 CHD 相关 PAH 的成人(APAH-CHD,N=185)。通过回归和 Kaplan-Meier 分析评估的结果包括血流动力学、内皮抑素随时间的变化和无移植存活率。在肺动脉内皮细胞和平滑肌细胞中评估内皮抑素分泌。与健康对照和 CHD 对照相比,PAH 患者的内皮抑素较高,APAH-CHD 患者的内皮抑素最高。在 APAH-CHD 中,内皮抑素与较短的 6 分钟步行距离和平均右心房压力增加有关。随着时间的推移,内皮抑素与较高的肺动脉压力和肺血管阻力指数、右心室扩张和功能障碍有关。随着时间的推移,内皮抑素随着血液动力学的改善而降低。内皮抑素与较差的无移植存活率相关。在基于 NT-proBNP(N 端前 B 型利钠肽)的生存分析中添加内皮抑素改善了风险分层,对具有不良结果的受试者进行了重新分类。内皮抑素主要由肺动脉内皮细胞分泌。
图 1. 按队列和 PAH 类型划分的内皮抑素浓度
研究结论:
内皮抑素与 APAH-CHD 的疾病严重程度、疾病改善和较差的生存相关。内皮抑素与 NT-proBNP 可改善风险分层,更好地预测不良结局。升高的内皮抑素与分流病变的关联表明内皮抑素可以由肺动脉流量和压力驱动。内皮抑素可以作为一种非侵入性预后标志物进行研究,特别是在 APAH-CHD 中。
文章出处:
Daly CM. Angiostatic Peptide, Endostatin, Predicts Severity in Pediatric Congenital Heart Disease-Associated Pulmonary Hypertension. J Am Heart Assoc. 2021 Oct 8:e021409. doi: 10.1161/JAHA.120.021409. Epub ahead of print. PMID: 34622662.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#内皮素#
95
#动脉高压#
80
#AHA#
81
#先天性#
90