Lancet:如何选择抗癌治疗时的静脉置管?
2021-07-21 Nebula MedSci原创
对于大多数接受SACT的癌症患者,PORT比Hickman和PICC更好用、更安全
Hickman型隧道导管(Hickman)、外周插入中心导管(PICC)和完全植入式端口(PORT)均用于通过中心静脉进行全身抗癌治疗(SACT)。本研究旨在比较三种设备的并发症发生率和成本,以确定这些设备对接受SACT的患者的可接受性、临床有效性和成本效益。
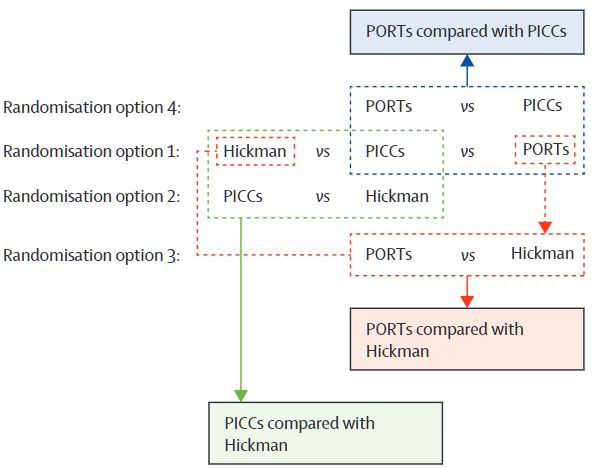
这是一项关于三种中心静脉通路装置的开放标签、多中心、随机对照试验:PICC vs Hickman(非劣效性;10%边界);PORT vs Hickman(优势性;15%边界);PORT vs PICC(优势性;15%边界)。招募了年满18岁的接受SACT(≥12周)治疗的实体或血液学恶性肿瘤患者,四种随机化分组选择:Hickman vs PICC vs PORT(2:2:1)、PICC vs Hickman(1:1)、PORT vs Hickman(1:1)和PORT vs PICC(1:1)。主要预后终点是拔管前、撤出研究前或随访1年内的并发症发生率(包括感染、静脉血栓、肺栓塞、不能回吸血液、器械故障和其他)。
研究设计
2013年11月8日-2018年2月28日,共筛查了2714位患者,其中1061位入组研究被随机分组:PICC vs Hickman(各212位);PORT(n=253) vs Hickman (n=303);PORT(n=147) vs PICC(n=199)。
各组对比细节
虽然观察到各组的并发症发生率差异小于10%,但可能是由于证据强度不足,PICC的非劣性未得到证实(比值比 [OR] 1.15 [95% CI 0.78–1.71])。PORT优于Hickman,对应的并发症发生率分别为29% vs 43%(OR 0.54 [95%CI 0.37-0.77])。PORT还优于PICC,并发症发生率分别为32% vs 47%(OR 0.52 [0.33–0.83])。
综上所述,对于大多数接受SACT的癌症患者,PORT比Hickman和PICC更好用、更安全。
原始出处:
Jonathan G Moss, et al. Central venous access devices for the delivery of systemic anticancer therapy (CAVA): a randomised controlled trial. The Lancet. July 20, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#静脉#
41
#Lancet#
64
#抗癌治疗#
77
顶刊就是不一样,质量很高,内容精彩!学到很多
67