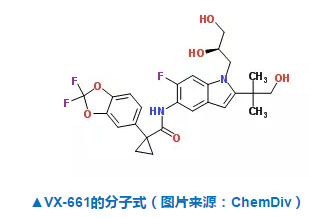
Free RadicBiol Med:谷胱甘肽缺乏会加重囊性纤维化疾病引起的支气管损害
2017-10-25 MedSci MedSci原创
CF(囊性纤维化)是一种侵犯多脏器的遗传性疾病。主要表现为外分泌腺的功能紊乱、粘液腺增生、分泌液粘稠、汗液氯化钠含量增高。临床上有肺脏、气道、胰腺、肠道、胆道、输精管、子宫颈等的腺管被粘稠分泌物堵塞所引起一系列症状,而以呼吸系统损害最为突出。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#DIC#
71
#Biol#
69
#囊性#
64
#支气管#
64
#Bio#
92
这个研究为CF治疗提供了新思路.谢谢研究者.谢谢梅斯医学!
109
#Med#
61
学习了.谢谢
113
学习了.谢谢分享
124