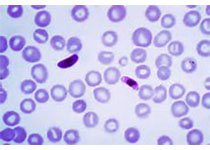
Leuk Lymphoma:利妥昔单抗存在不良反应 新模式识别高风险患者
2017-08-15 梁舒瑶 环球医学资讯
2017年11月,发表在《Leuk Lymphoma》的一项由意大利科学家进行的374名患者的回顾性、多中心研究,发现了静脉注射利妥昔单抗后发生的药物不良反应,在恶性血液肿瘤中比自身免疫性疾病更常见,并且可通过临床和实验室参数的结合来预测。
原始出处:
D'Arena G, Simeon V, Laurenti L,et al. Adverse drug reactions after intravenous rituximab infusion are more common in hematologic malignancies than in autoimmune disorders and can be predicted by the combination of few clinical and laboratory parameters: results from a retrospective, multicenter study of 374 patients.Leuk Lymphoma. 2017 Nov;58(11):2633-2641. doi: 10.1080/10428194.2017.1306648. Epub 2017 Apr 3.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#高风险#
67
#利妥昔#
67
#不良反应#
71
#lymphoma#
75
学习了,谢谢作者分享!
78