J Clin Periodonto:牙周炎和视网膜微循环在动脉粥样硬化中的风险
2015-03-14 MedSci译 MedSci原创
J Clin Periodonto:牙周炎和视网膜微循环在动脉粥样硬化中的风险关键词:牙周炎 视网膜 微循环在发达国家,牙周疾病(PDs)几乎影响了50%的30岁以上人群。PDs是细菌引起的炎症性疾病,累及支持牙齿的软硬组织。牙根表面的菌斑生物膜是始动因子,破坏牙周结缔组织和牙槽骨。如果不治疗PDs,病情继续发展,最终结果是牙齿脱落。慢性牙周炎是PDs最常见的一种类型,与许多全身状况有关,包括血
在发达国家,牙周疾病(PDs)几乎影响了50%的30岁以上人群。PDs是细菌引起的炎症性疾病,累及支持牙齿的软硬组织。牙根表面的菌斑生物膜是始动因子,破坏牙周结缔组织和牙槽骨。如果不治疗PDs,病情继续发展,最终结果是牙齿脱落。
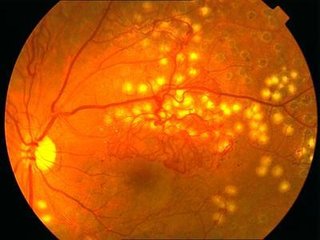
目的:本次横断面研究的目的是为了探讨牙周炎是否与视网膜微循环(预测心血管疾病的指标)的改变有关。
材料和方法:本研究包括了来自ARIC的457例52岁及以上的患者。作为视网膜中心动脉/静脉(CRAE/CRVE)测量和总结视网膜血管的参数。使用CDC/AAP定义来判断牙周炎。采用多变量线性回归分析模型来评估CRAE、CRVE以及牙周炎之间的关系。
结果:未发现CRAE与牙周状况有关。然而,CRVE与中毒牙周炎则成正相关,并有显著地统计学关联。校正了混杂因素后,健康—牙龈炎组平均CRVE(±标准差)为187.0+17.2μm,中、重度牙周炎组,则分别为188.5±16.3μm和191.6±16.8μm(p=0.04)。仅考虑糖尿病参与者(n=66)而不考虑非糖尿病参与者时,结果是一致的。
结论:重度牙周炎与2型糖尿病患者的较大的视网膜小静脉直径有关。需要进一步研究来探讨糖尿病对牙周炎和视网膜微循环关系的影响。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












好文章,还会关注
96
#PE#
76
#微循环#
65
#粥样硬化#
90
#视网膜#
103
#牙周#
103